Accurate Error Estimation and Statistical Analysis of Diffusion Coefficients: A Guide for Biomedical Researchers
This article provides a comprehensive guide for researchers and drug development professionals on the accurate estimation and statistical analysis of diffusion coefficients.
Accurate Error Estimation and Statistical Analysis of Diffusion Coefficients: A Guide for Biomedical Researchers
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on the accurate estimation and statistical analysis of diffusion coefficients. It covers foundational principles, from Fickian diffusion to the Einstein relation, and explores diverse methodological approaches, including molecular dynamics simulations, Taylor dispersion, and ATR-FTIR. A strong emphasis is placed on troubleshooting common errors in statistical analysis and data fitting, such as those arising from MSD analysis and model misspecification. Finally, the article presents a framework for the validation and comparative analysis of diffusion data across different experimental and computational techniques, highlighting applications in critical areas like drug delivery and medical diagnostics. The goal is to empower scientists to produce more reliable and reproducible diffusion data for biomedical applications.
Core Principles: Understanding Diffusion and the Critical Role of Error
Your Questions Answered
This guide addresses common challenges researchers face when determining diffusion coefficients, with a special focus on statistical best practices for robust error estimation.
FAQ 1: What is the most reliable method to calculate a diffusion coefficient from a molecular dynamics (MD) simulation?
The most common and recommended method is the Mean Squared Displacement (MSD) approach [1] [2]. For a three-dimensional, isotropic system, the diffusion coefficient D is calculated from the slope of the MSD plot at long time intervals using the Einstein relation:
$$MSD(t) = \langle [\mathbf{r}(t) - \mathbf{r}(0)]^2 \rangle = 6Dt$$
Therefore,
$$D = \frac{1}{6} \times \text{slope}(MSD)$$ [1] [2]
- Best Practice: Ensure your simulation is long enough that the MSD plot is linear in the diffusive regime. At short times, motion may be ballistic (MSD ~ t²), and other sub-diffusive regimes may exist before normal diffusion (MSD ~ t) is observed [2].
- Alternative Method: The Velocity Autocorrelation Function (VACF) is another valid technique [1] [2]: $$D = \frac{1}{3} \int_{0}^{\infty} \langle \mathbf{v}(0) \cdot \mathbf{v}(t) \rangle dt$$
FAQ 2: Why is my MSD plot not a perfect straight line, and how does this affect error estimation?
An MSD plot is never a perfect straight line because it is derived from finite simulation data with inherent statistical noise [3]. Using simple Ordinary Least Squares (OLS) regression on MSD data is problematic because the data points are serially correlated and heteroscedastic (having unequal variances) [3]. This leads to:
- Statistical Inefficiency: The estimate of D has a larger-than-necessary statistical uncertainty [3].
- Underestimated Uncertainty: The standard error calculated by OLS significantly underestimates the true uncertainty in D [3], which can cause overconfidence in the result.
FAQ 3: What advanced statistical methods provide better error estimates for diffusion coefficients?
To overcome the limitations of OLS, use regression methods that account for the true correlation structure of the MSD data.
- Generalized Least-Squares (GLS) and Bayesian Regression: These methods use the full covariance matrix of the MSD, which describes the correlations between data points and their changing variances [3]. This leads to estimates of D that are statistically more efficient (have smaller uncertainty) and provide a more accurate estimate of the statistical error [3].
- Maximum Likelihood Estimation (MLE): This is another powerful optimization method that determines the set of parameters (like D) that make the observed data most probable [4]. It performs exceptionally well, particularly with short trajectories or when localization errors are significant, and is known to determine the correct distribution of diffusion coefficients [4].
FAQ 4: How do I correct for finite-size effects in my simulation box?
The diffusion coefficient measured in a simulation with Periodic Boundary Conditions (DPBC) is influenced by hydrodynamic interactions with periodic images. You can apply a correction to estimate the value for an infinite system [2]:
$$D{\text{corrected}} = D{\text{PBC}} + \frac{2.84 k_{B}T}{6 \pi \eta L}$$
Where kB is Boltzmann's constant, T is temperature, η is the shear viscosity of the solvent, and L is the length of the cubic simulation box [2].
Experimental Protocols for Robust Diffusion Estimation
The following workflow outlines the key steps for calculating and statistically validating a diffusion coefficient from an MD trajectory, integrating the FAQ solutions.
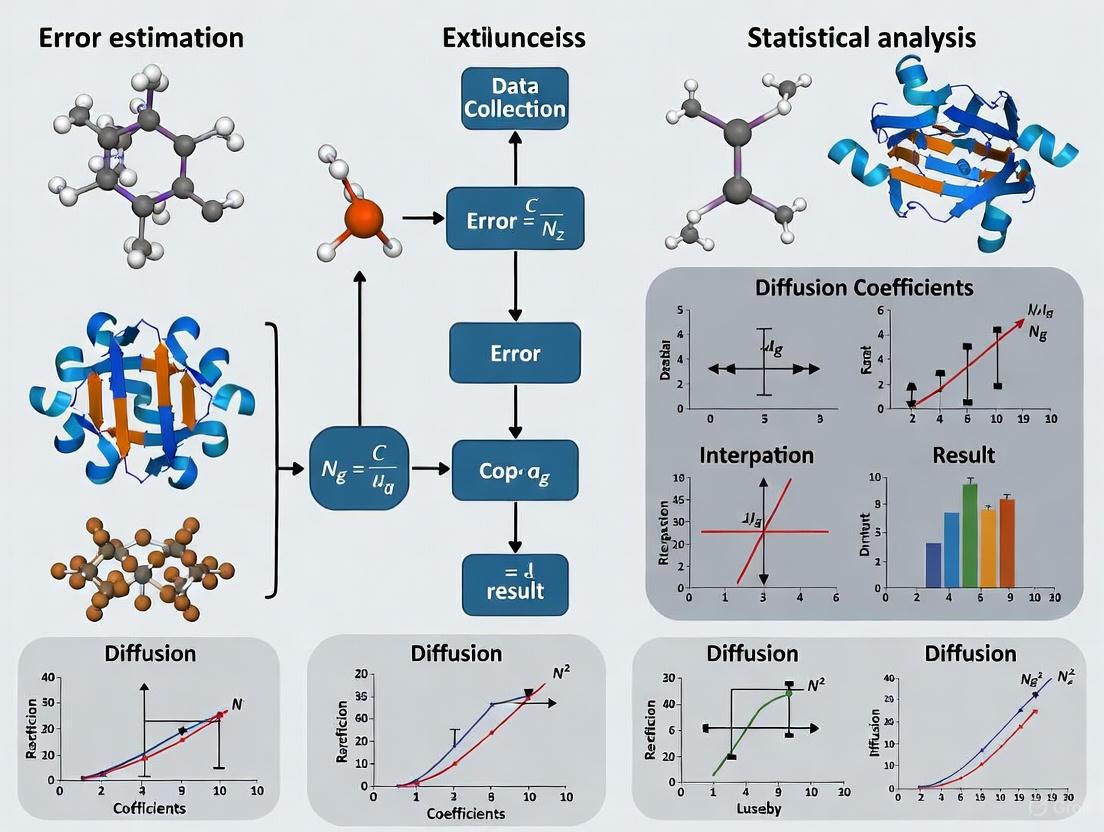
Diagram: Workflow for Estimating Diffusion Coefficients.
Step 1: Compute the MSD Calculate the MSD from your trajectory by averaging over all particles and multiple time origins [3] [2]. The general 3D formula is: $$MSD(t) = \langle | \mathbf{r}(t') - \mathbf{r}(t' + t) |^2 \rangle$$ where the angle brackets denote an average over all particles and time origins t' [2].
Step 2: Inspect the MSD and Identify the Diffusive Regime Plot the MSD against time. Do not fit the entire curve. Identify the long-time linear region where normal diffusion occurs and use this for fitting [2].
Step 3: Check for Normal Diffusion Before proceeding, it is crucial to verify that the system exhibits normal diffusion. Use a statistical test, such as a Kolmogorov-Smirnov test, to check if the observed dynamics are consistent with normal diffusion or if they are anomalous [5].
Step 4: Fit the MSD with an Appropriate Algorithm Fit the linear portion of the MSD curve to obtain the slope and thus the diffusion coefficient. The choice of fitting method directly impacts the reliability of your error estimate [3] [4].
Step 5: Apply Finite-Size Correction Use the Yeh-Hummer correction formula [2] provided in FAQ 4 to adjust your calculated D for the finite size of your simulation box.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Computational Tools for Diffusion Coefficient Research
| Tool / Reagent | Function / Purpose | Key Application Note |
|---|---|---|
| kinisi (Python package) | Implements Bayesian regression for estimating D from MSD with accurate uncertainty [3]. | The preferred tool to avoid underestimated errors from OLS fitting. Uses a parametrized covariance model. |
| Generalized Least-Squares (GLS) | A statistically efficient regression method that accounts for correlations in MSD data [3]. | Provides a point estimate equal to the Bayesian mean. Requires a model for the MSD covariance matrix. |
| Maximum Likelihood Estimation (MLE) | Estimates parameters by maximizing the probability of the observed trajectory [4]. | Superior to MSD-analysis for short trajectories or large localization errors. |
| Finite-Size Correction | Analytical formula to correct for system size effects in PBC simulations [2]. | Essential for obtaining the macroscopic diffusion coefficient from finite-sized simulations. |
| 3,3'-Difluorobenzaldazine | 3,3'-Difluorobenzaldazine, CAS:1049983-12-1; 15332-10-2, MF:C14H10F2N2, MW:244.245 | Chemical Reagent |
| 1,4-Butanediol mononitrate-d8 | 1,4-Butanediol mononitrate-d8, CAS:1261398-94-0, MF:C4H9NO4, MW:143.168 | Chemical Reagent |
Table: Comparison of Diffusion Coefficient Estimation Methods
| Method | Statistical Efficiency | Uncertainty Estimation | Key Assumptions Met? | Recommended Use Case |
|---|---|---|---|---|
| Ordinary Least Squares (OLS) | Low | Significantly underestimates true uncertainty [3] | No (assumes independent, identically distributed data) [3] | Not recommended for final analysis. |
| Weighted Least Squares (WLS) | Moderate (better than OLS) | Still underestimates uncertainty [3] | No (accounts for heteroscedasticity but not correlation) [3] | A moderate improvement over OLS. |
| Generalized Least-Squares (GLS) | High (theoretically maximal) [3] | Accurate when correct covariance is used [3] | Yes (accounts for both heteroscedasticity and correlation) [3] | Optimal choice when accurate covariance matrix is known. |
| Bayesian Regression | High (theoretically maximal) [3] | Accurate (provides full posterior distribution) [3] | Yes (accounts for both heteroscedasticity and correlation) [3] | Optimal for reliable estimation and uncertainty quantification from a single trajectory. |
| Maximum Likelihood (MLE) | High (asymptotically optimal) [4] | Accurate [4] | Handles localization error and motion blur | Best for single-particle tracking with experimental noise [4]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary sources of uncertainty when determining diffusion coefficients from through-diffusion experiments?
The estimation of diffusion parameters (effective diffusion coefficient De, porosity ε, and adsorption coefficient KD) is affected by several experimental biases. Key sources of uncertainty include [6]:
- The presence of filters and tubing: Filters holding the clay sample in place and connecting tubing create dead volumes that can distort the estimation of diffusive fluxes and sample porosity.
- Sampling events: The periodic sampling of the low-concentration reservoir to measure tracer accumulation alters the concentration gradient across the diffusion cell, which is the fundamental driver of diffusion.
- O-ring and filter setups: The physical setup for delivering solutions to the clay packing can introduce unexpected errors in the applied concentration boundary conditions. A consistent numerical modeling approach that simultaneously accounts for all these factors, rather than treating them in isolation, is recommended for accurate parameter estimation [6].
Q2: How can I improve the accuracy of anomalous diffusion exponent (α) estimates from short single-particle trajectories?
For short trajectories, two major sources of error are significant statistical variance and systematic bias [7].
- For Variance: Employ ensemble-based estimation. By analyzing a collection of multiple particle trajectories collectively, you can characterize the method-specific noise and use this information to perform a shrinkage correction, which optimally combines information from individual trajectories with ensemble statistics.
- For Bias: Use time–ensemble averaged mean squared displacement (TEA-MSD). This approach provides a more reliable and length-invariant method for characterizing diffusion behavior, enabling accurate correction of systematic bias in the ensemble mean, particularly for normal and super-diffusive regimes [7].
Q3: What is the difference between "real-world uncertainty" and "statistical uncertainty"?
These terms reflect different scopes of what "uncertainty" means [8]:
- Statistical Uncertainty is a narrow, technically defined concept focused on repeatability. It answers the question: "If I repeated the data collection process many times, how much would my results vary just by chance?" It is often quantified by measures like the standard error.
- Real-World Uncertainty is a broader concept encompassing all "unknowns." This includes statistical uncertainty but also factors like measurement errors, unaccounted-for model simplifications, and systemic biases. A statistical margin of error often understates the total real-world uncertainty [8].
Q4: What framework can help ensure I've considered all major types of model-related uncertainty?
A useful "sources of uncertainty" framework breaks model-related uncertainty into four key areas [9]:
- Response Variable: Uncertainty in the primary variable you are trying to explain or predict (e.g., measurement error).
- Explanatory Variables: Uncertainty in the predictor variables (e.g., measurement error, missing data).
- Parameter Estimates: Uncertainty in the model's parameter values (e.g., standard errors, confidence intervals).
- Model Structure: Uncertainty about the model's mathematical form itself (e.g., whether a relationship is linear or non-linear). An audit of scientific papers showed that while no field fully considers all sources, this framework provides a checklist to improve the completeness of uncertainty reporting [9].
Troubleshooting Guides
Issue 1: Inconsistent Diffusion Parameters Across Replicate Experiments
Potential Cause: Uncorrected Experimental Biases. The raw data from your through-diffusion experiments may be influenced by the physical setup of your apparatus, leading to a flawed estimation of De and ε [6].
Solution: Implement a Comprehensive Numerical Model.
- Action: Use a reactive transport code (e.g., CrunchClay with its CrunchEase interface) to model the entire experimental system directly, rather than just converting data into diffusive fluxes.
- Protocol:
- Model the Full Geometry: Explicitly include the dimensions and properties of the filters, tubing, and O-rings in your numerical model.
- Simulate Sampling Events: Model the actual process of sampling from the low-concentration reservoir, which changes its volume and concentration over time.
- Direct Data Fitting: Fit the model parameters directly to the measured (radio)tracer concentrations in the source and reservoir, rather than to the calculated fluxes. This approach more accurately accounts for the impact of the experimental biases on the final results [6].
Issue 2: High Variance and Bias in Anomalous Diffusion Exponents from Short Trajectories
Potential Cause: Inherent Statistical Limitations of Short Time Series. The variance of the exponent estimate α is inversely proportional to the trajectory length T: Var[α] ∠1/T. For very short trajectories, this variance becomes substantial. Furthermore, finite-length effects can introduce systematic bias [7].
Solution: Apply Ensemble-Based Correction Methods.
- Action: Leverage information from multiple trajectories to correct estimates from individual ones.
- Protocol for Variance Correction [7]:
- Calculate the estimated exponent α̂i for each trajectory i in your ensemble using your chosen method (e.g., TA-MSD).
- Compute the ensemble mean (μ̄α) and total observed variance (σ̂²total).
- Estimate the variance of your estimation method (σ²TAMSD) using a known relationship (e.g., for TA-MSD with specific lags, σ²TAMSD ≈ 0.9216/T).
- The corrected estimate for a trajectory can be derived by optimally combining the individual estimate with the ensemble mean, based on the relative magnitudes of the method variance and the true ensemble variance.
Protocol for Bias Correction [7]:
- Use the Time-Ensemble Averaged MSD (TEA-MSD), which averages displacement data across both time and multiple trajectories. This provides a more robust and less biased characterization of the diffusion process for short trajectories compared to single-trajectory TA-MSD.
The tables below summarize key quantitative data on measurement performance and uncertainty from the search results.
Table 1: Multi-Institution Performance of Apparent Diffusion Coefficient (ADC) Measurements in a Phantom Study [10]
| Performance Metric | Result | Description |
|---|---|---|
| Mean ADC Bias | < 0.01 × 10-3 mm²/s (0.81%) | Average difference between measured and ground-truth ADC. |
| Isocentre ADC Error Estimate | 1.43% | Error estimate at the center of the measurement. |
| Short-Term Repeatability | < 0.01 × 10-3 mm²/s (1%) | Intra-scanner variability over a short time. |
| Reproducibility | 0.07 × 10-3 mm²/s (9%) | Inter-scanner variability across multiple institutions. |
Table 2: Uncertainty Framework for Model-Related Uncertainty [9]
| Source of Uncertainty | Element in a Model | Examples of Uncertainty |
|---|---|---|
| Response Variable | The focal variable being explained/predicted. | Measurement or observation error. |
| Explanatory Variables | Variables used to explain the response. | Measurement error, missing data. |
| Parameter Estimates | Estimated model parameters (e.g., intercept, slope). | Standard errors, confidence intervals. |
| Model Structure | The mathematical form of the model itself. | Choice of a linear vs. a non-linear model. |
Experimental Protocols & Workflows
Protocol 1: Deriving Diffusion Parameters from Through-Diffusion Experiments
This protocol details the methodology for interpreting through-diffusion data to determine De, ε, and KD, while correcting for experimental biases [6].
1. Experimental Setup:
- A clay sample of thickness Ls and cross-sectional area A is packed into a diffusion cell.
- A high-concentration reservoir with tracer concentration c0 is maintained on one side.
- A low-concentration reservoir is kept near zero by periodic replacement and sampling.
2. Data Collection:
- Over time tn, sample the low-concentration reservoir, measuring the tracer concentration cL(tn) and volume VL(tn) at each interval.
- Calculate the cumulated amount of tracer Q(tn) in the low-concentration reservoir: Q(tn) = Σ cL(tn) VL(tn) [6].
- The experimental tracer diffusive flux Fexp(tn) is evaluated using a numerical derivative (e.g., backward difference): Fexp(tn) = [Q(tn) - Q(tn-1)] / [(tn - tn-1) A] [6].
3. Numerical Interpretation with Bias Correction:
- Instead of directly fitting an ideal model to Fexp, use a reactive transport code to create a digital twin of the experiment.
- The model should incorporate the geometry of filters, tubing volumes, and simulate reservoir volume changes during sampling events.
- The model solves Fick's second law, often in a form simplified for homogeneous media [6]:
∂c/∂t = [D<sub>e</sub> / (ε + Ï<sub>d</sub>K<sub>D</sub>)] * (∂²c/∂x²) - Model parameters (De, ε, KD) are optimized by fitting the model's output directly to the measured reservoir concentration data, thereby accounting for biases in the system.
The following workflow diagrams the process of estimating parameters while accounting for different uncertainty sources.
Diagram 1: Through-diffusion parameter estimation workflow.
Protocol 2: Ensemble-Based Estimation of Anomalous Diffusion Exponents
This protocol is designed for analyzing single-particle tracking (SPT) data to estimate the anomalous diffusion exponent α for cases where trajectories are short, a common scenario in live-cell imaging [7].
1. Data Preprocessing:
- Obtain a set of M two-dimensional particle trajectories, each of length T coordinates: (X(t), Y(t)).
2. Single-Trajectory Exponent Estimation (TA-MSD Method):
- For each trajectory i, compute the Time-Averaged Mean Squared Displacement (TA-MSD) for a range of lag times Ï„ [7]:
TA-MSD(τ) = (1/(T-τ)) * Σ [ (X(t+τ) - X(t))² + (Y(t+τ) - Y(t))² ](sum from t=1 to t=T-τ) - Perform a linear regression of
log(TA-MSD(τ))againstlog(τ). - The slope of this regression line is the estimate for the anomalous diffusion exponent, α̂i, for trajectory i.
3. Ensemble-Based Correction:
- Calculate Ensemble Statistics: Compute the mean (μ̄α) and total variance (σ̂²total) of all α̂i estimates.
- Apply Variance Correction: Use the known relationship between estimation variance and trajectory length for your method (e.g., for TA-MSD, Var[α̂] ≈ 0.9216 / T for lags {1,2,3,4}) to refine the individual estimates by shrinking them toward the ensemble mean.
- Apply Bias Correction: For a more robust estimate of the ensemble's true α, calculate the Time-Ensemble Averaged MSD (TEA-MSD), which averages displacement data across all trajectories and time points, and then perform the log-log regression on this consolidated dataset.
The following flowchart visualizes this ensemble-based correction methodology.
Diagram 2: Ensemble-based correction workflow for anomalous diffusion analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Diffusion Experimentation
| Item | Function / Relevance |
|---|---|
| Room-Temperature DWI Phantom | A standardized object containing a reference material with a known ground-truth Apparent Diffusion Coefficient (ADC). It is used for quality assurance and multi-scanner validation studies without the complexity of an ice-water setup [10]. |
| MR-Readable Thermometer | Critical for accurately measuring the temperature of a phantom or sample during diffusion experiments. Enables correction of measured ADC values to their ground-truth values based on temperature-dependent diffusion properties [10]. |
| Reactive Transport Code (e.g., CrunchClay) | A numerical software platform that models the coupled processes of chemical reaction and transport (e.g., diffusion) in porous media. Essential for implementing advanced interpretation models that correct for experimental biases [6]. |
| Graphical User Interface (e.g., CrunchEase) | A tool that automates the creation of input files, running of simulations, and extraction of results for complex models. Makes advanced reactive transport modeling accessible to experimentalists without a deep background in computational science [6]. |
| Fractional Brownian Motion (fBm) Simulator | A computational tool to generate synthetic trajectories of anomalous diffusion. Used for method validation, testing the performance of estimation algorithms, and training machine learning models under controlled conditions [7]. |
| Ethyl 5-methyl-1H-pyrazole-3-carboxylate | Ethyl 5-methyl-1H-pyrazole-3-carboxylate, CAS:886495-75-6, MF:C7H10N2O2, MW:154.17 g/mol |
| D(+)-Galactosamine hydrochloride | D(+)-Galactosamine hydrochloride, CAS:1886979-58-3, MF:C6H14ClNO5, MW:215.63 g/mol |
The Importance of Accurate Diffusion Data in Drug Development and Biomaterial Design
Your Troubleshooting Guide for Diffusion Data Challenges
This guide addresses common experimental issues in diffusion coefficient estimation, providing targeted solutions to enhance the reliability of your data in drug and biomaterials research.
Problem: High Uncertainty in Estimated Diffusion Coefficients from MD Simulations
- Question: "My molecular dynamics (MD) simulations produce mean squared displacement (MSD) data with significant noise, leading to high uncertainty in my diffusion coefficient (D*). How can I obtain a more reliable and statistically efficient estimate?"
- Solution: Replace Ordinary Least Squares (OLS) regression with a method that accounts for the statistical nature of MSD data.
- Root Cause: MSD data points are serially correlated (each point depends on the previous one) and heteroscedastic (their variance changes over time). OLS assumes data points are independent and identically distributed, violating these assumptions and leading to inefficient estimates and a significant underestimation of the statistical uncertainty [3].
- Recommended Protocol: Employ Bayesian regression or Generalized Least Squares (GLS) using an analytically derived covariance matrix, Σ, which models the correlations and changing variances in the MSD data [3].
- Procedure:
- Calculate the observed MSD from your trajectory.
- Parametrize a model covariance matrix, Σ′, from your observed data. This matrix approximates the true covariance structure of an equivalent system of freely diffusing particles.
- Use this covariance matrix in a Bayesian regression framework to sample the posterior distribution of linear models (m = 6Dt + c) that fit the MSD data.
- The mean of the posterior distribution for D provides a statistically efficient point estimate, and the spread of the distribution accurately quantifies its uncertainty [3].
- Tools: This method is implemented in the open-source Python package
kinisi[3].
Problem: Weak Signal and Fluorescence Interference in Experimental Diffusion Measurements
- Question: "When measuring molecular diffusion in biological tissues or hydrogels using Raman spectroscopy, the signal is weak and overwhelmed by background fluorescence and autofluorescence. How can I improve the signal-to-noise ratio?"
- Solution: Utilize Stimulated Raman Scattering (SRS) microscopy instead of spontaneous Raman spectroscopy [11].
- Root Cause: Spontaneous Raman scattering is an inherently weak process, where only 1 in 10⸠photons is inelastically scattered. In complex, biological samples, this weak signal is often obscured by a strong fluorescent background [11].
- Recommended Protocol: SRS employs two pulsed lasers (a pump and a Stokes beam) that coherently excite molecular vibrations. This process amplifies the Raman signal by several orders of magnitude and is inherently free from fluorescence interference [11].
- Procedure:
- Sample Preparation: Use a model compound with a distinct Raman signature in a silent region of the spectrum. A robust choice is deuterated glucose (d7-glucose), as its C-D stretching vibration is spectrally isolated from native C-H vibrations [11].
- Data Acquisition: Construct a sample holder (e.g., a thin glass cuvette) containing your hydrogel or tissue slice. Add the deuterated glucose solution on top and use the SRS system to monitor the C-D band intensity over time and space [11].
- Data Analysis: The SRS signal is proportional to the concentration of the probe molecule. By measuring the spatiotemporal concentration profile, you can calculate the diffusion coefficient, even in highly scattering samples like tissues [11].
Frequently Asked Questions (FAQs)
How can I generate data for drug discovery when experimental diffusion data is sparse or missing?
Answer: Diffusion models, a class of generative artificial intelligence, can create high-quality synthetic data to address data sparsity.
- Application: A novel diffusion GNN model called Syngand can generate synthetic ligand and pharmacokinetic data end-to-end [12].
- Methodology: These models learn the underlying distribution of existing, sparse datasets. Researchers can then sample from this learned distribution to generate novel, synthetic data points that span multiple datasets, enabling the exploration of research questions that would otherwise be limited by data availability [12].
- Utility: This synthetically generated data has been shown to improve the performance of downstream prediction tasks, such as regression models for properties like solubility (AqSolDB) and toxicity (LD50, hERG) [12].
My molecule's diffusion in biological tissue doesn't follow classical Fickian laws. What does this mean?
Answer: Observing non-Fickian or anomalous diffusion often indicates more complex, biologically relevant transport mechanisms.
- Interpretation: While mass transport within simple hydrogel matrices may follow Fickian diffusion, diffusion within tissues is often more complex due to interactions with cellular structures, binding events, and the heterogeneous nature of the extracellular matrix [11].
- Investigation Path: Use advanced diffusion measurement techniques like SRS (see above) to accurately characterize these complex profiles. Then, model the data using more sophisticated frameworks beyond the simple Einstein relation to gain insights into the specific transport barriers and mechanisms at play [11].
The Scientist's Toolkit: Essential Reagents & Computational Tools
This table details key materials and software essential for advanced diffusion studies.
| Item Name | Function/Application | Key Characteristics |
|---|---|---|
| Deuterated Glucose (d7-glucose) | A model small molecule for tracing diffusion in biomaterials and tissues using SRS [11]. | C-D bond provides a distinct Raman signature in a spectrally "silent" region, free from interference [11]. |
| Stimulated Raman Scattering (SRS) Microscope | Measures molecular diffusion in highly scattering or fluorescent samples (e.g., tissues, hydrogels) [11]. | Amplifies Raman signals; eliminates fluorescence background; provides high-contrast, real-time chemical imaging [11]. |
kinisi Python Package |
Accurately estimates self-diffusion coefficients (D*) and their uncertainties from MD simulation trajectories [3]. | Implements Bayesian regression with a model covariance matrix for high statistical efficiency from a single simulation [3]. |
| Syngand Model | A diffusion-based generative model that creates synthetic ligand and pharmacokinetic data [12]. | Addresses data sparsity in AI-based drug discovery by generating data for multi-dataset research questions [12]. |
| N-Valeryl-D-glucosamine | N-Valeryl-D-glucosamine, MF:C11H21NO6, MW:263.29 g/mol | Chemical Reagent |
| Burnettramic acid A aglycone | Burnettramic acid A aglycone, MF:C35H61NO7, MW:607.9 g/mol | Chemical Reagent |
Experimental & Statistical Workflows
The following diagrams outline core methodologies for obtaining accurate diffusion data.
SRS Diffusion Measurement
Bayesian D* Estimation
FAQs on Fundamental Concepts
1.1 What is the fundamental difference between MSD and ADC?
The Mean Squared Displacement (MSD) and Apparent Diffusion Coefficient (ADC) are related but distinct metrics for quantifying particle motion. The MSD is a direct measure of the deviation of a particle's position over time, representing the spatial extent of its random motion. It is calculated as the average of the squared distance a particle travels over a given time lag [13]. In contrast, the ADC is a derived parameter that represents the measured diffusion coefficient in a voxel or region of interest, reflecting the average mobility of water molecules as influenced by the local tissue microenvironment and experimental conditions [14]. The ADC is essentially the diffusion coefficient calculated from MRI measurements, and it is "apparent" because it is influenced by numerous biophysical factors and experimental setups, unlike the theoretical diffusion coefficient of pure water [14].
1.2 In what types of experiments should I use MSD versus ADC?
Your choice of metric depends on your imaging modality and experimental goal.
- Use MSD primarily in Single Particle Tracking (SPT) experiments. These are typically optical microscopy techniques (e.g., interferometric scattering microscopy) where you follow the trajectory of individual particles, such as molecules in a cell membrane, over time [15]. MSD analysis is applied to the reconstructed particle path.
- Use ADC in Diffusion Magnetic Resonance Imaging (MRI) studies. This is the standard metric for quantifying water diffusion in clinical and biological research MRI. It provides a voxel-averaged measure of water mobility, which is sensitive to tissue cellularity, microstructure, and integrity [16] [14] [17].
1.3 My ADC values are inconsistent across repeated scans. What are the common sources of this variability?
Inconsistent ADC measurements are a well-documented challenge, often stemming from both technical and biological factors [18].
- Scanner-related Factors: Significant variations in ADC values can occur between different MRI scanner manufacturers, models, and even across scanners of the same model. Instabilities in the gradient system or the reference voltage can also lead to fluctuations [19] [18].
- Sequence and Protocol Choices: The selection of b-values (the diffusion-weighting parameters) greatly influences the ADC. Using a 2-point method (e.g., b=0, b=800 s/mm²) is common but can be less consistent than a multi-point b-value technique [18]. The imaging sequence itself (e.g., single-shot echo-planar imaging vs. turbo spin echo) can also introduce variability [18].
- Sample Environment: Temperature variations can affect both the diffusion of water molecules and the performance of electronic components in the scanner, leading to ADC drift [19]. Fat suppression techniques in bone marrow imaging have also been shown to yield significantly different ADC values [16].
Troubleshooting Guides
Troubleshooting MSD Measurements in Single Particle Tracking
| Symptom | Possible Cause | Solution |
|---|---|---|
| Erroneously detected subdiffusion or overestimated diffusion coefficients [15]. | Localization uncertainty is overlooked, especially problematic at short time lags where particle displacement is comparable to the error [15]. | Use an analysis pipeline that explicitly accounts for localization error, such as the Apparent Diffusion Coefficient (ADC) analysis in the TRAIT2D software [15]. |
| Spurious results at short time ranges [15]. | Motion blurring inherent in SPT due to particle movement during frame acquisition [15]. | Ensure your analysis method corrects for motion blur. Select an appropriate number of data points for MSD fitting, as relying on very first points can be misleading [15]. |
| Inability to track particles accurately at high framerates. | Conventional tracking algorithms may not be optimized for long, uninterrupted, high-speed trajectories [15]. | Employ tracking algorithms designed for high sampling rates that favor strong spatial and temporal connections between consecutive frames [15]. |
Experimental Protocol for Robust MSD Analysis:
- Data Acquisition: Acquire particle trajectories using a high-speed microscopy technique (e.g., iSCAT) [15].
- Particle Localization: Identify particle positions with sub-pixel precision using an algorithm like the radial symmetry centre approach [15].
- Trajectory Linking: Construct trajectories using a linking algorithm suitable for high-frame-rate data [15].
- MSD Calculation: Compute the MSD for each trajectory using the formula:
MSD(n∙Δt) = 1/(N-n) ∙ Σ [r((i+n)∙Δt) - r(i∙Δt)]², wherer(t)is the position at timet,Δtis the time between frames, andnis the time lag index [13]. - Model Fitting: Fit the MSD plot to an appropriate diffusion model (e.g., Brownian, confined). Use statistical model selection to identify the best model and be cautious of over-interpreting short-time-lag data [15].
Troubleshooting ADC Measurements in Diffusion MRI
| Symptom | Possible Cause | Solution |
|---|---|---|
| Fluctuating ADC readings, even with a stable phantom [19] [18]. | System noise from electromagnetic interference, power supply noise, or crosstalk [19]. | Use decoupling capacitors near the ADC's power supply pins. Employ a stable, precision external reference voltage source instead of the scanner's internal reference [19] [18]. |
| Significant differences in ADC values between scanners or sites [18]. | Lack of protocol standardization, including different b-values, sequences, and scanners [18]. | Implement standardized, multicenter imaging protocols. Use a liquid isotropic phantom for cross-calibration and quality assurance across all scanners [18]. |
| ADC values that drift over time or with changes in ambient temperature [19]. | Temperature variations affecting the sample and scanner electronics [19]. | Use components with low temperature coefficients. Monitor scanner room temperature. For longitudinal studies, schedule scans at a consistent time of day. |
| Clipped or low-resolution ADC measurements [19]. | Mismatch between the input signal's range and the ADC's input range [19]. | Use signal conditioning circuits to scale the input signal to match the ADC's input range optimally. |
| Incorrect signal representation or aliasing artifacts [19]. | Insufficient sampling rate violating the Nyquist theorem [19]. | Increase the sampling rate to at least 2.5 times the highest frequency in the input signal. Use an anti-aliasing filter. |
Experimental Protocol for Robust ADC Measurement in MRI:
- Phantom Calibration: For multicenter studies or longitudinal quality control, use a standardized liquid isotropic phantom to assess reproducibility across MRI systems [18].
- Sequence Selection: Consider using a Turbo Spin Echo (TSE) sequence over single-shot Echo-Planar Imaging (ssEPI) if possible, as TSE has been shown to yield more homogeneous ADC values [18].
- b-value Selection: Employ a multi-point b-value technique (e.g., b=0, 50, 500, 1000, 1500 s/mm²) instead of a 2-point method for more consistent and accurate ADC fitting [18].
- ADC Calculation: The ADC is calculated per voxel by fitting the signal decay across different b-values to the equation:
S_b = S_0 * exp(-b * ADC), whereS_bis the signal intensity with diffusion weightingb, andS_0is the signal without diffusion weighting [14].
Essential Research Reagent Solutions
| Item | Function in Experiment |
|---|---|
| Liquid Isotropic Phantom | A standardized reference material used to calibrate MRI scanners, assess the reproducibility of ADC measurements across different platforms and sites, and control for variables not present in living tissue [18]. |
| Fat Suppression Pre-pulses (STIR, SSRF) | Techniques used in MRI to suppress the signal from fat tissue, which is crucial for obtaining accurate ADC measurements of water diffusion in tissues like bone marrow. Different techniques can yield different ADC values [16]. |
| Decoupling Capacitors | Passive electronic components placed near the power supply pins of ADC units to filter out high-frequency noise, ensuring a clean power source and reducing fluctuating readings [19]. |
| Anti-aliasing Filter | A low-pass filter applied before the ADC sampling process to attenuate signal frequencies higher than half the sampling rate, preventing aliasing artifacts and incorrect signal representation [19]. |
| TRAIT2D Software | An open-source Python library for tracking and analyzing single particle trajectories. It provides localization-error-aware analysis pipelines for calculating MSD and ADC, and includes simulation tools [15]. |
Workflow Visualization
MSD Analysis Workflow
ADC Measurement Workflow
Frequently Asked Questions (FAQs)
1. What is the practical difference between the variance and the covariance?
Variance measures how much a single random variable spreads out from its own mean. In contrast, covariance measures how two variables change together; a positive value indicates they tend to move in the same direction, while a negative value suggests they move in opposite directions [20]. In the context of estimating a diffusion coefficient, you might calculate the variance of repeated measurements at a single time point. You would examine covariance to understand if the measurement error at one time point is related to the error at another.
2. How is a variance-covariance matrix estimated from my experimental data?
For a dataset with p variables and n independent observations, the unbiased estimate for the variance-covariance matrix Q is calculated using the formula [20]:
Q = 1/(n-1) * Σ (x_i - x̄)(x_i - x̄)^T
where x_i is the i-th observation vector and x̄ is the sample mean vector. The factor n-1 (Bessel's correction) ensures the estimate is unbiased. For diffusion data, each variable might represent the measured particle position at a different time, and this matrix would quantify the variability and co-variability of these positions across time.
3. My statistical software reports a confidence interval. What is the correct interpretation?
A 95% confidence interval means that if you were to repeat the entire data collection and interval calculation process many times, approximately 95% of the calculated intervals would contain the true population parameter [21]. It is incorrect to say there is a 95% probability that a specific calculated interval contains the true value; the true value is fixed, and the interval either contains it or it does not [21]. For example, a 95% CI for a diffusion coefficient means that the method used to create the interval is reliable 95% of the time over the long run.
4. When should I use a prediction interval instead of a confidence interval?
Use a confidence interval to estimate an unknown population parameter, like a true mean diffusion coefficient. Use a prediction interval to express the uncertainty in predicting a future single observation [21]. A confidence interval for a diffusion coefficient estimates the true coefficient itself, while a prediction interval would bracket where you expect the next measured coefficient from a new experiment to fall.
Troubleshooting Guides
Issue 1: High Variance in Estimated Diffusion Coefficients
Problem: Calculated diffusion coefficients from replicate experiments show high variance, making the results unreliable.
Diagnosis: This often stems from uncontrolled environmental factors or measurement system noise.
Solution:
- Step 1: Control Experimental Conditions. Ensure temperature, solvent viscosity, and sample purity are consistent across all replicates. Uncontrolled fluctuations directly contribute to observed variance.
- Step 2: Calibrate Instrumentation. Verify the calibration of all measurement equipment (e.g., microscopes, light scatterers). High instrument noise inflates variance.
- Step 3: Increase Sample Size. If the inherent variability is high, a larger number of experimental replicates (
n) will lead to a more precise estimate of the mean, as the standard error decreases with the square root ofn[21].
Issue 2: Interpreting the Variance-Covariance Matrix Output
Problem: A statistical package has produced a variance-covariance matrix, but you are unsure how to interpret its values.
Diagnosis: The diagonal and off-diagonal elements have distinct meanings.
Solution:
- Step 1: Read the Diagonals. The diagonal elements are the variances of each individual parameter estimate. A large value indicates high uncertainty for that specific parameter.
- Step 2: Read the Off-Diagonals. The off-diagonal elements are the covariances between two parameter estimates. A large absolute value (positive or negative) indicates that the errors in estimating those two parameters are related.
- Step 3: Check for Correlation. High covariance can sometimes make a model numerically unstable. If two parameters have a very high covariance, it may suggest they are not both independently needed in your model.
Issue 3: Confidence Interval is Too Wide
Problem: The calculated confidence interval for your parameter of interest (e.g., a mean) is too broad to be useful for drawing conclusions.
Diagnosis: The interval width is driven by the variability in the data and the sample size.
Solution:
- Step 1: Investigate Sources of Variability. Analyze your experimental process for sources of excessive noise. The solution to Issue 1 may also help here.
- Step 2: Increase Sample Size. This is the most direct way to narrow a confidence interval. The width of the interval is proportional to
1/√n[21]. Doubling your sample size reduces the interval width by about 30%. - Step 3: Check for Outliers. Examine your data for anomalous points that could be artificially inflating the measured variance. Use diagnostic plots or robust statistical methods if outliers are present [20].
Essential Formulas and Data
Key Formulas for Error Estimation
Table 1: Core formulas for variance, covariance, and confidence intervals.
| Concept | Formula | Description |
|---|---|---|
| Sample Variance (s²) | s² = Σ(xi - x̄)² / (n - 1) [22] [20] |
Measures the average squared deviation from the mean. Unbiased estimator of population variance. |
| Sample Covariance | Cov(X,Y) = Σ(xi - x̄)(yi - ȳ) / (n - 1) [20] |
Measures the direction of the linear relationship between two variables. |
| 95% CI for Mean (μ) | x̄ ± t*(s / √n) [21] |
Provides a range of plausible values for the population mean. t* is the critical value from the t-distribution with n-1 degrees of freedom. |
| Variance-Covariance Matrix (Sample Estimate) | Q = 1/(n-1) * Σ (xi - x̄)(xi - x̄)^T [20] |
A square matrix where diagonals are variances and off-diagonals are covariances. |
Statistical Software Toolkit
Table 2: Common statistical software packages and their applications in research.
| Software | Primary Users | Key Features & Highlights | Potential Limitations |
|---|---|---|---|
| SPSS | Social Sciences, Health Sciences, Marketing [23] | Intuitive menu-driven interface; easy data handling and missing data management [23]. | Absence of some robust regression methods; limited complex data merging [23]. |
| Stata | Economics, Political Science, Public Health [23] | Powerful for panel, survey, and time-series data; strong data management; integrates matrix programming [23]. | Limited graph flexibility; only one dataset in memory at a time [23]. |
| SAS | Financial Services, Government, Life Sciences [23] | Handles extremely large datasets; powerful for data management; many specialized components [23]. | Graphics can be cumbersome; steep learning curve for new users [23]. |
| R | Data Science, Bioinformatics, Finance [23] | Vast array of statistical packages; high-quality, customizable graphics (e.g., ggplot2); free and open-source [23]. | Command-line driven, requiring programming knowledge; steeper initial learning curve [23]. |
| (1R,2S,3R)-Aprepitant | (1R,2S,3R)-Aprepitant, CAS:221350-96-5, MF:C23H21F7N4O3, MW:534.4 g/mol | Chemical Reagent | Bench Chemicals |
| (Tyr0)-C-peptide (human) | (Tyr0)-C-peptide (human), MF:C138H220N36O50, MW:3183.4 g/mol | Chemical Reagent | Bench Chemicals |
Experimental Protocol: Estimating a Diffusion Coefficient and its Confidence Interval
Objective: To determine the diffusion coefficient (D) of a fluorescently labeled molecule in a solution and report its value with a 95% confidence interval.
1. Materials and Reagents
- Purified Molecule of Interest: The analyte whose diffusion is being measured.
- Fluorescent Label: A stable, bright fluorophore that does not alter the molecule's hydrodynamic properties.
- Imaging Buffer: A chemically defined buffer to maintain pH and ionic strength.
- Coverslip Chamber: A sample holder for microscopy.
- Confocal Microscope or Light Scattering Instrument: Equipment capable of tracking particle movement.
2. Methodology
- Step 1: Sample Preparation. Dilute the labeled molecule to an appropriate concentration in the imaging buffer to minimize particle interaction. Load the sample into the imaging chamber.
- Step 2: Data Acquisition. Using a single-particle tracking or dynamic light scattering protocol, record the trajectories or intensity fluctuations of the molecules. Ensure data is collected for a sufficient duration to capture the diffusion behavior. Repeat this process for a minimum of
n = 30independent experimental replicates. - Step 3: Calculate Diffusion Coefficients. For each replicate
i, fit the mean squared displacement (MSD) to the relationMSD(Ï„) = 4D_i Ï„(for 2D diffusion) to obtain an estimate of the diffusion coefficientD_ifor that replicate. - Step 4: Statistical Summary. Calculate the sample mean (
DÌ„) and sample standard deviation (s) of thenestimated diffusion coefficients. - Step 5: Construct Confidence Interval. Using
D̄,s, andn, calculate the 95% confidence interval asD̄ ± t*(s / √n), wheret*is the critical value from a t-distribution withn-1degrees of freedom [21].
Visualizations
Statistical Analysis Workflow
Relationship Between Sample Size and Confidence Interval
From Theory to Practice: Methods for Estimating Diffusion Coefficients
Troubleshooting Guide: Common MD Simulation Errors
Frequently Encountered Errors in GROMACS
Q: What does the error "Out of memory when allocating" mean and how can I resolve it?
A: This error occurs when the program cannot assign the required memory for the calculation [24]. Solutions include:
- Reducing the number of atoms selected for analysis.
- Processing a shorter trajectory length.
- Verifying unit consistency (e.g., confusion between Ångström and nm can create a system 10³ times larger than intended) [24].
- Using a computer with more memory [24].
Q: How should I address "Residue 'XXX' not found in residue topology database" from pdb2gmx?
A: This means your selected force field lacks parameters for residue 'XXX' [24]. To resolve this:
- Verify the residue name in your PDB file matches the name in the force field's residue database.
- If no database entry exists, you cannot use pdb2gmx and must:
- Parameterize the residue yourself.
- Find a topology file for the molecule and include it in your topology.
- Use a different force field with parameters for this residue [24].
Q: What causes "Found a second [defaults] directive" in grompp and how do I fix it?
A: This error occurs when the [defaults] directive appears more than once in your topology or force field files [24]. To fix it:
- Locate and comment out or delete the duplicate
[defaults]section in the secondary file. - Avoid mixing force fields, as this often causes the issue [24].
Q: What is the correct way to include position restraints for multiple molecules?
A: Position restraint files must be included immediately after their corresponding [moleculetype] block [24].
Correct Implementation:
Common Mistakes in MD Simulation Setup
Q: What are critical checks before starting a production MD simulation?
A: Before launching your simulation, always [25]:
- Check 1: Match temperature and pressure coupling parameters to those used in your NVT and NPT equilibration steps.
- Check 2: Use the auto-fill input path feature when building upon a previous equilibration to prevent manual path errors.
- Check 3: Tune advanced parameters (via the "All..." button) for custom constraints or force settings.
- Check 4: Save your configuration and consider exporting parameter sets for version control.
Q: Why is structure preparation so important and what should I check?
A: Simulation quality depends directly on your starting structure [26]. Proper preparation involves checking for:
- Missing atoms or residues.
- Steric clashes and unrealistic geometries.
- Correct protonation states at your simulation pH.
- Appropriate tautomers [26]. Use tools like pdbfixer or H++ to assist with preparation [26].
Q: How do I choose an appropriate time step?
A: An inappropriate timestep is a common mistake [26].
- A too large timestep causes numerical instability, unrealistic atom movement, and simulation failure.
- A too small timestep wastes computational resources without improving accuracy [26]. Balance accuracy and efficiency by considering your force field, bonded constraints, atomic masses, and use of virtual sites [26].
Q: How can I avoid artefacts from Periodic Boundary Conditions (PBC)?
A: PBCs can cause molecules to appear split across box boundaries [26]. To prevent analysis errors:
- Use built-in correction tools before analysis (e.g.,
gmx trjconvin GROMACS with the-pbc nojumpflag orcpptrajin AMBER) [26] [27]. - Always make molecules "whole" before calculating metrics like RMSD, hydrogen bonds, or distances [26].
Troubleshooting Guide: MSD Analysis for Diffusion Coefficients
Common Problems in MSD Analysis
Q: My MSD values are orders of magnitude too large. What is the most likely cause?
A: This often indicates a unit mismatch between the coordinate units in your trajectory and the expected units of the MSD analysis tool [28]. Verify the units of your input data (e.g., nm vs. μm) and apply consistent scaling. Ensure your trajectory is in unwrapped coordinates to avoid artificial suppression of diffusion from periodic boundary wrapping [27].
Q: How many MSD points should I use to fit the diffusion coefficient D?
A: The optimal number of MSD points (p_min) for fitting is critical and depends on the reduced localization error x = σ²/DΔt (where σ is localization uncertainty, D is diffusion coefficient, and Δt is frame duration) [29].
- When
x << 1(small localization error), use the first two MSD points. - When
x >> 1(significant localization error), a larger number of points is needed [29]. The optimal numberp_mindepends on bothxandN(total trajectory points) and can be determined theoretically [29].
Q: What defines a reliable MSD curve for calculating diffusivity?
A: A reliable MSD curve should have a linear segment at intermediate time lags [27]. Exclude:
- Short time lags: May exhibit ballistic, non-diffusive motion.
- Long time lags: Suffer from poor averaging and increased statistical error [29] [27]. Use a log-log plot to identify the linear region, which should have a slope of 1 [27].
Q: Why are replicate simulations important for MSD analysis?
A: A single trajectory may not represent the system's full thermodynamic behavior or may be trapped in a local minimum [26]. Multiple replicates:
- Provide better statistical sampling of conformational space.
- Increase confidence in observed behaviors and calculated diffusion coefficients.
- Help distinguish true diffusion from artifacts or rare events [26].
Important: When combining MSDs from multiple replicates, average the MSDs themselves (combined_msds = np.concatenate(...)) rather than concatenating trajectory coordinates, which creates artificial jumps [27].
Quantitative Data for MSD Analysis
Table 1: Key Parameters for Optimal MSD Fitting [29]
| Parameter | Symbol | Effect on MSD Analysis | Practical Consideration |
|---|---|---|---|
| Reduced Localization Error | x = σ²/DΔt |
Determines the optimal number of MSD points for fitting. | Use theoretical expression to find p_min based on your x and N. |
| Localization Uncertainty | σ |
Increases variance of initial MSD points. | Dominates error when x >> 1. Calculate from PSF and photon count [29]. |
| Trajectory Length | N |
Longer trajectories improve averaging. | For small N, p_min may be as large as N. |
| Frame Duration | Δt |
Shorter intervals better capture motion. | Affects x. Balance with signal-to-noise. |
Table 2: MSD Fitting Guidelines for Diffusion Coefficient Calculation [29] [27]
| Condition | Optimal Number of Fitting Points | Fitting Method | Expected Outcome |
|---|---|---|---|
Small Localization Error (x << 1) |
First 2 points | Unweighted least squares | Reliable estimate of D. |
Significant Localization Error (x >> 1) |
p_min (theoretically determined) |
Unweighted or weighted least squares | Requires more points for reliable D. |
| General Case | Linear portion of MSD curve | Linear regression on MSD ~ 2dDÏ„ |
Slope gives 2dD, where d is dimensionality. |
Experimental Protocols
Protocol 1: System Preparation and Equilibration for MD
- Structure Preparation: Obtain initial coordinates (e.g., from PDB). Check for missing atoms/residues, assign correct protonation states, and correct steric clashes using tools like pdbfixer [26].
- Topology Generation: Use
pdb2gmxor similar to generate topology within your chosen force field. Ensure all residues are recognized [24]. - System Assembly: Solvate the protein in an appropriate water box and add ions to neutralize the system and achieve desired concentration.
- Energy Minimization: Use steepest descent or conjugate gradient minimisation to remove bad contacts and relax the system [26].
- Equilibration:
- NVT Equilibration: Equilibrate the system at constant temperature (e.g., 300 K) using a thermostat (e.g., Berendsen, Nosé-Hoover).
- NPT Equilibration: Further equilibrate at constant pressure (e.g., 1 bar) using a barostat (e.g., Parrinello-Rahman). Verify stabilization of temperature, pressure, density, and potential energy before proceeding to production [25] [26].
Protocol 2: Calculating Diffusion Coefficient from MSD
- Trajectory Requirement: Ensure your trajectory is in unwrapped coordinates (use
gmx trjconv -pbc nojumpfor GROMACS) [27]. - Compute MSD: Calculate the ensemble-averaged MSD using the Einstein formula. For efficient computation, use an FFT-based algorithm if available [27].
MSD = msd.EinsteinMSD(u, select='all', msd_type='xyz', fft=True) - Identify Linear Region: Plot MSD vs. lag time (Ï„) on a log-log plot. Identify the intermediate time-lag region where the slope is approximately 1 [27].
- Fit MSD to Einstein Relation: Within the linear region, perform a linear fit:
MSD(Ï„) = 2dDÏ„, wheredis the dimensionality [27].linear_model = linregress(lagtimes[start_index:end_index], msd[start_index:end_index]) - Calculate D: Extract the slope and compute the diffusion coefficient:
D = slope / (2 * d)[27]. - Repeat and Average: Perform this analysis on multiple independent simulation replicates and average the results for a statistically robust measurement [26] [27].
Diagrams and Workflows
MD Setup and Analysis Workflow
MSD Analysis for Diffusion Coefficient
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for MD Simulations
| Tool/Software | Primary Function | Key Application in Research |
|---|---|---|
| GROMACS | Molecular dynamics package | High-performance MD simulation engine for running production simulations [24]. |
| pdb2gmx | Topology generator | Creates molecular topologies from coordinate files, assigning force field parameters [24]. |
| grompp | Preprocessor | Processes topology and parameters to create a run input file [24]. |
| MDAnalysis | Trajectory analysis | Python library for analyzing MD trajectories, including MSD calculations [27]. |
| EinsteinMSD | MSD analysis | Specific class in MDAnalysis for computing mean squared displacement via Einstein relation [27]. |
| CHARMM36m | Force field | Optimized for proteins, provides parameters for bonded and non-bonded interactions [26]. |
| GAFF2 | Force field | General Amber Force Field for organic molecules and drug-like compounds [26]. |
| gmx trjconv | Trajectory processing | Corrects periodic boundary conditions and unwraps coordinates for accurate MSD analysis [26] [27]. |
| Aromadendrin 7-O-rhamnoside | Aromadendrin 7-O-rhamnoside, MF:C21H22O10, MW:434.4 g/mol | Chemical Reagent |
| Methiothepin Mesylate | Methiothepin Mesylate, CAS:74611-28-2, MF:C21H28N2O3S3, MW:452.7 g/mol | Chemical Reagent |
Bayesian Regression for Optimal Estimation from MSD Data
Quantitative tracking of particle motion using live-cell imaging is a powerful approach for understanding the transport mechanisms of biological molecules, organelles, and cells. However, inferring complex stochastic motion models from single-particle trajectories presents significant challenges due to sampling limitations and inherent biological heterogeneity. Bayesian regression provides a powerful statistical framework for analyzing Mean Squared Displacement (MSD) data, enabling researchers to obtain optimal estimates of diffusion coefficients while rigorously quantifying uncertainty. This approach is particularly valuable in pharmaceutical development and biological research where understanding molecular mobility is crucial for drug mechanism studies and cellular process characterization.
Unlike traditional frequentist methods, Bayesian approaches formally incorporate prior knowledge and provide direct probability statements about parameters of interest, such as diffusion coefficients. This methodology allows researchers to continuously update their beliefs as new experimental data accumulates, creating a virtuous cycle of knowledge refinement in diffusion coefficients research. The Bayesian framework is especially suited for handling the complex error structures often encountered in MSD data analysis, including measurement errors, model inadequacies, and intrinsic stochasticity of biological systems.
Key Concepts and Theoretical Framework
Foundation of Bayesian Inference for MSD Data
The Bayesian approach to MSD-based analysis employs multiple-hypothesis testing of a general set of competing motion models based on particle mean-square displacements. This method automatically classifies particle motion while properly accounting for sampling limitations and correlated noise, appropriately penalizing model complexity according to Occam's Razor to avoid over-fitting. The core of Bayesian inference revolves around three fundamental components:
Prior Probability Distribution (P(θ)): Represents initial beliefs about parameters (e.g., diffusion coefficients) before observing current experimental data. Priors can be informative (based on previous studies or expert knowledge) or non-informative (minimally influential, allowing data to dominate conclusions) [30].
Likelihood (P(Data|θ)): Quantifies how probable the observed MSD data are, given particular values for the parameters θ. It represents the information contributed by the current experimental measurements [30].
Posterior Probability Distribution (P(θ|Data)): Represents updated beliefs about parameters after combining prior knowledge with experimental MSD data. This is calculated using Bayes' theorem: P(θ|Data) = [P(Data|θ) × P(θ)] / P(Data) [30].
Bayesian Workflow for MSD Analysis
The following diagram illustrates the systematic Bayesian framework for MSD data analysis:
Bayesian MSD Analysis Workflow
Research Reagent Solutions for MSD Experiments
Table 1: Essential research reagents and computational tools for Bayesian MSD analysis
| Reagent/Tool | Function | Application Context |
|---|---|---|
| Bayesian Logistic Regression Model (BLRM) | Connects drug doses to side effect risks through logistic regression; starts with prior beliefs about dose safety and updates with new data [31]. | Phase I clinical trials testing new therapies for safety and dosing; adaptive trial designs that use all available information for dose adjustments. |
| Bayesian Age-Period-Cohort (BAPC) Models | Projects future disease burden trends using Bayesian framework with Integrated Nested Laplace Approximation (INLA) for efficient computation [32]. | Forecasting global burden of musculoskeletal disorders; modeling disease trends in postmenopausal women using Global Burden of Disease data. |
| Markov Chain Monte Carlo (MCMC) Algorithms | Enables sampling from posterior distributions without calculating marginal likelihoods directly; includes Metropolis-Hastings, Gibbs Sampling, and Hamiltonian Monte Carlo [30]. | Parameter estimation for complex diffusion models; uncertainty quantification in pharmaceutical process development and characterization. |
| Stan Modeling Platform | State-of-the-art platform for statistical modeling using Hamiltonian Monte Carlo (HMC) and No-U-Turn Sampler (NUTS) for efficient parameter space exploration [30]. | Building complex hierarchical models for MSD data; high-dimensional parameter estimation in biological diffusion studies. |
| Bayesian Finite Element Model Updating | Builds accurate numerical models for structural systems while quantifying associated model uncertainties in a Bayesian framework [33]. | Uncertainty quantification in model parameters; addressing modeling errors, parameter errors, and measurement errors in complex systems. |
| Power Prior Modeling | Formal methodology for incorporating historical data or external information into new trials using weighted prior distributions [34]. | Borrowing strength from previous MSD experiments; integrating historical control data in confirmatory clinical trials. |
Troubleshooting Common Experimental Issues
Model Selection and Validation Challenges
Table 2: Troubleshooting guide for Bayesian MSD analysis
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Poor MCMC Convergence | High autocorrelation between samples; inappropriate proposal distribution; insufficient burn-in period [30]. | Use Hamiltonian Monte Carlo (HMC) or NUTS algorithms; increase effective sample size; run multiple chains with different initial values. | Check trace plots and Gelman-Rubin statistic (R-hat); ensure R-hat < 1.05 for all parameters. |
| Overly Influential Priors | Too narrow prior distributions; strong subjective beliefs dominating likelihood [30]. | Conduct prior sensitivity analysis; use weakly informative priors; apply power priors with carefully chosen weights [34]. | Specify priors based on previous relevant studies; use domain expertise to justify prior choices. |
| Model Misspecification | Incorrect likelihood function; inappropriate motion model for biological process; missing covariates [35]. | Implement posterior predictive checks; compare multiple competing models using Bayes factors; use Bayesian model averaging. | Perform exploratory data analysis; consider multiple model structures (Brownian, anomalous diffusion, directed motion). |
| Inadequate Uncertainty Quantification | Ignoring model form errors; not accounting for measurement errors; underestimating parameter uncertainty [33]. | Use hierarchical Bayesian models; include error terms for measurement precision; employ Bayesian model updating techniques. | Classify uncertainty sources (aleatoric vs. epistemic); use robust likelihood formulations. |
| Computational Limitations | High-dimensional parameter spaces; complex likelihood functions; large datasets [36]. | Implement variational inference methods; use integrated nested Laplace approximations (INLA); employ surrogate modeling. | Start with simplified models; use efficient data structures; consider distributed computing approaches. |
Data Quality and Preprocessing Issues
Problem: Noisy MSD Trajectories Affecting Parameter Estimates
Experimental particle tracking data often contains substantial noise from various sources, including limited photon counts in fluorescence microscopy, thermal drift, and biological heterogeneity. This noise can significantly impact diffusion coefficient estimates and lead to misclassification of motion types.
Solution Protocol:
- Implement Bayesian Denoising: Apply Bayesian smoothing algorithms that incorporate prior knowledge about expected motion characteristics while accounting for measurement noise properties.
- Hierarchical Modeling: Use multi-level hierarchical models that separate measurement error from biological variability, allowing proper uncertainty propagation through the analysis.
- Model Comparison Framework: Employ systematic Bayesian approaches for multiple-hypothesis testing of competing motion models that automatically penalize model complexity to avoid overfitting [35].
- Validation with Simulations: Generate synthetic trajectories with known parameters using the posterior predictive distribution to verify that the analysis recovers true parameter values.
Experimental Protocols for Bayesian MSD Analysis
Comprehensive Protocol for Diffusion Coefficient Estimation
The following diagram outlines the complete experimental workflow for Bayesian MSD analysis:
MSD Experimental Analysis Pipeline
Step-by-Step Procedure:
Experimental Design and Data Collection
- Acquire particle tracking data with appropriate temporal and spatial resolution
- Record relevant experimental conditions (temperature, buffer composition, cell type)
- Collect sufficient trajectories for statistical power (typically 50-100 per condition)
Bayesian Model Specification
- Define prior distributions for diffusion coefficients based on literature or pilot studies
- Specify likelihood function accounting for measurement noise and motion type
- Consider multiple competing models (Brownian motion, anomalous diffusion, directed transport)
Computational Implementation
- Implement MCMC sampling using platforms like Stan, Nimble, or PyMC
- Run multiple chains with dispersed starting values
- Monitor convergence using Gelman-Rubin statistics (R-hat) and effective sample size
Posterior Analysis and Validation
- Extract posterior distributions for parameters of interest
- Calculate credible intervals for diffusion coefficients
- Perform posterior predictive checks to assess model adequacy
- Compare models using Bayes factors or information criteria
Protocol for Uncertainty Quantification in MSD Analysis
Objective: Properly characterize and quantify different sources of uncertainty in MSD-based diffusion coefficient estimates.
Procedure:
Classify Uncertainty Sources:
- Aleatoric uncertainty: Intrinsic randomness in particle motion
- Epistemic uncertainty: Limited knowledge about model parameters
- Model form uncertainty: Potential misspecification of physical models
- Measurement uncertainty: Experimental noise in trajectory tracking [33]
Implement Hierarchical Bayesian Models:
- Separate particle-level variability from population-level trends
- Include random effects for biological replicates
- Account for measurement precision using error-in-variables models
Bayesian Model Averaging:
- Compute posterior model probabilities for competing motion models
- Weight parameter estimates by model probabilities
- Obtain robust diffusion estimates that account for model uncertainty
Advanced Bayesian Techniques for MSD Data
Bayesian Model Selection Framework
The Bayesian approach provides a natural framework for comparing multiple competing models of particle motion. By computing posterior model probabilities, researchers can objectively select the simplest model that adequately explains the observed MSD data, following the principle of Occam's Razor. This systematic approach to multiple-hypothesis testing automatically penalizes model complexity to avoid overfitting, which is particularly important when analyzing complex motion patterns from single-particle trajectories [35].
The model evidence, also known as the marginal likelihood, serves as a key quantity for Bayesian model comparison. This integral averages the likelihood function over the prior distribution of parameters, automatically incorporating a penalty for model complexity. For MSD data analysis, this approach enables researchers to distinguish between different modes of motion, such as Brownian diffusion, confined motion, directed transport, or anomalous diffusion, based on probabilistic reasoning rather than arbitrary thresholding.
Incorporating Prior Knowledge in Pharmaceutical Applications
In drug development contexts, Bayesian methods formally incorporate existing knowledge into clinical trial design, analysis, and decision-making. The Bayesian Logistic Regression Model (BLRM) exemplifies this approach by combining prior beliefs about dose safety with real-time patient data to guide dose selection in Phase I trials [31]. This methodology creates a feedback loop where each patient's experience informs safer and more effective doses for subsequent participants, maximizing the efficiency of clinical development while maintaining patient safety.
The Bayesian framework is particularly valuable for dose escalation studies, where prior information about compound toxicity and pharmacokinetics can be formally incorporated using informative prior distributions. This approach allows for more efficient trial designs with smaller sample sizes while maintaining rigorous safety standards, addressing ethical imperatives to expose the fewest patients to potentially ineffective or unsafe treatment regimens [37].
Frequently Asked Questions (FAQs)
Q1: How does Bayesian analysis of MSD data differ from traditional least-squares fitting?
A1: Bayesian methods provide several advantages over traditional least-squares approaches:
- They quantify uncertainty in parameter estimates using credible intervals rather than just point estimates
- They formally incorporate prior knowledge through prior distributions
- They enable direct probability statements about parameters (e.g., "There is a 95% probability that the diffusion coefficient lies between X and Y")
- They automatically penalize model complexity through the marginal likelihood, reducing overfitting
- They handle hierarchical data structures naturally, accounting for both within-trajectory and between-trajectory variability [30] [35]
Q2: What are the computational requirements for Bayesian MSD analysis?
A2: Bayesian analysis typically requires more computational resources than traditional methods:
- MCMC sampling may require thousands of iterations for convergence
- Complex models with many parameters benefit from parallel computing
- Memory requirements scale with dataset size and model complexity
- Efficient implementations using platforms like Stan, Nimble, or PyMC can significantly reduce computation time
- For very large datasets, variational inference methods provide faster approximations to the posterior [30] [36]
Q3: How should I choose prior distributions for diffusion coefficient analysis?
A3: Prior selection should be guided by:
- Previous studies on similar systems
- Physical constraints (diffusion coefficients must be positive)
- Pilot experiments or preliminary data
- Sensitivity analysis to assess prior influence
- For exploratory analyses, use weakly informative priors that regularize estimates without strongly influencing results
- Document and justify all prior choices in your methodology [30] [34]
Q4: How can I validate my Bayesian MSD model?
A4: Comprehensive model validation includes:
- Posterior predictive checks: simulating new data from the posterior and comparing to observed data
- Cross-validation: assessing model performance on held-out data
- Convergence diagnostics: ensuring MCMC chains have properly explored the posterior
- Residual analysis: checking for systematic patterns in model errors
- Comparison with alternative models using Bayes factors or information criteria
- Recovery studies: testing whether the model can recover known parameters from simulated data [35] [33]
Q5: Can Bayesian methods handle heterogeneous populations in single-particle tracking?
A5: Yes, Bayesian methods are particularly well-suited for heterogeneous populations:
- Finite mixture models can identify subpopulations with different diffusion characteristics
- Hierarchical models naturally account for both within-group and between-group variability
- Nonparametric Bayesian methods automatically infer the number of subpopulations from the data
- Model comparison techniques help determine whether multiple populations are justified by the data
- These approaches provide a more realistic representation of biological systems where heterogeneity is common [35]
FAQs: Core Principles and Data Interpretation
Q1: What is the fundamental principle behind Taylor Dispersion Analysis? Taylor Dispersion Analysis (TDA) is a technique for determining the diffusion coefficients of molecules in solution. It is based on the dispersion of a narrow solute plug injected into a carrier solvent flowing under laminar (Poiseuille) conditions within a capillary. The parabolic velocity profile of the flow causes solute molecules at the center to move faster than those near the walls. This, combined with radial diffusion of the molecules, leads to the axial dispersion of the solute plug. The extent of this dispersion, which can be quantified by the temporal variance of the resulting concentration profile (Taylorgram), is inversely related to the solute's diffusion coefficient. From the diffusion coefficient (D), the hydrodynamic radius (Rh) can be calculated using the Stokes-Einstein equation [38] [39].
Q2: For a polydisperse sample, what does the calculated hydrodynamic radius represent? For a polydisperse sample or mixture, a single fit to the Taylorgram provides a weighted average diffusion coefficient, and thus a weighted average hydrodynamic radius. For mass-sensitive detectors (like UV/Vis absorbance), this average is a mass-based average [39]. Studies have shown that for a monomodal sample with relatively low polydispersity, this average is typically very close to the weight-average diffusion coefficient (Dw). However, for highly polydisperse or bimodal samples, the value can differ significantly from other averages, such as the z-average obtained from Dynamic Light Scattering (DLS) [40].
Q3: What are the key advantages of TDA compared to other sizing techniques? TDA offers several distinct advantages [39] [41]:
- Absence of Calibration: The method is absolute and does not require calibration standards for size determination.
- Insensitivity to Dust: Measurements are performed in a capillary, making the technique insensitive to dust particles; sample filtration is typically not required.
- Minimal Sample Consumption: Very small sample volumes (a few nanoliters) are injected.
- Wide Size Range: Effective for hydrodynamic radii from approximately 0.2 nm to 300 nm.
- No Bias Towards Large Species: Provides a mass-based distribution, avoiding the intensity-based bias of DLS which can overemphasize large aggregates.
- Fast Analysis: Experiments are typically rapid.
Q4: How does TDA handle and quantify sample aggregation? In a monodisperse sample, the Taylorgram is a symmetrical Gaussian peak. The presence of aggregates leads to a deviation from this Gaussian shape because the Taylorgram becomes a sum of the Gaussian profiles of the individual species (e.g., monomer, dimer, aggregate). The broader peak width indicates the presence of larger, slower-diffusing species [38] [39]. Advanced data processing methods, such as Constrained Regularized Linear Inversion (CRLI), can be used to deconvolute the experimental Taylorgram and extract the probability density function of the diffusion coefficients, thereby quantifying the relative proportions of the different populations in the sample [39].
Troubleshooting Guides
Non-Gaussian Taylorgram Peaks
A non-Gaussian peak shape often indicates an issue with the sample or the experimental conditions.
- Symptom: Tailing or fronting peaks, or peaks with shoulders.
- Potential Causes and Solutions:
- Sample Polydispersity/Aggregation: This is a physicochemical property of the sample, not an experimental error. Use advanced data analysis (e.g., CRLI) to resolve the different populations [39].
- Sample-Surface Interactions: Adsorption of the solute to the capillary walls can cause peak tailing.
- Solution: Consider using a different capillary material (e.g., coated capillaries) or modifying the buffer conditions (e.g., pH, ionic strength) to minimize interaction.
- Injected Sample Plug Profile: An imperfect initial sample plug can distort the peak.
- Solution: Ensure consistent and clean injection procedures. The use of a two-window detection method can help correct for a non-ideal initial plug shape [38].
Inconsistent Diffusion Coefficient Measurements
When replicate measurements show high variability, consider the following aspects.
- Symptom: High variance in calculated D or Rh values across repeated runs.
- Potential Causes and Solutions:
- Unstable Flow: Fluctuations in the driving pressure will alter the dispersion process.
- Solution: Verify the stability of the pressure regulator or syringe pump. Ensure there are no leaks in the fluidic path.
- Temperature Fluctuations: The diffusion coefficient and solvent viscosity are highly temperature-sensitive.
- Solution: Perform experiments in a temperature-controlled environment and allow sufficient time for the instrument and capillary to equilibrate.
- Sample Preparation Variability: Inconsistent sample dissolution or handling can lead to changes in concentration or aggregation state.
- Solution: Standardize sample preparation protocols. For proteins and sensitive biomolecules, centrifuge samples briefly before injection to remove any pre-existing large aggregates.
- Unstable Flow: Fluctuations in the driving pressure will alter the dispersion process.
Failure to Meet Validity Conditions
The core equations of TDA are valid only under specific conditions. Violating these conditions leads to systematic errors.
- Symptom: Measured diffusion coefficients are inaccurate.
- Potential Causes and Solutions:
- Radial Equilibrium Not Reached: The analysis requires that the observation time is long enough for solute molecules to sample the entire flow velocity profile via radial diffusion.
- Solution: Ensure the residence time ( t0 ) meets the criterion: ( t0 >> \frac{Rc^2}{D} ), where ( Rc ) is the capillary radius. A more precise condition for a 3% tolerable error is ( t0 > 1.7 \frac{Rc^2}{D} ) [39].
- Significant Axial Diffusion: The model assumes that Taylor dispersion is the dominant spreading mechanism, not simple axial diffusion.
- Solution: The Peclet number (Pe) should be sufficiently high. For a 3% error, the condition is ( \text{Pe} = \frac{2UR_c}{D} > 28.7 ) [39]. This can be achieved by adjusting the flow velocity (U) or selecting a capillary with an appropriate radius.
- Radial Equilibrium Not Reached: The analysis requires that the observation time is long enough for solute molecules to sample the entire flow velocity profile via radial diffusion.
The following workflow and troubleshooting diagram outlines the key experimental steps and a logical path for diagnosing common issues.
Essential Experimental Protocols
Protocol: Determining Diffusion Coefficient via the Two-Window Method
This protocol outlines the standard method for determining the diffusion coefficient (D) and hydrodynamic radius (Rh) of a monodisperse sample, which minimizes errors from the initial sample injection profile [38] [39].
- Capillary Calibration: Precisely measure the internal radius (( R_c )) of the capillary and the exact distance (( L )) between the two detection windows.
- System Equilibration: Flush the capillary with run buffer. Apply the desired operating pressure and allow the system to stabilize until a stable baseline is achieved. Ensure the instrument is at a constant temperature.
- Sample Injection: Inject a small nanoliter-volume plug of the sample into the capillary.
- Data Acquisition: Under continuous laminar flow, record the absorbance (or other concentration-sensitive signal) versus time at both detection windows. These profiles are the Taylorgrams.
- Peak Fitting: Fit each Taylorgram to a Gaussian model (Equation 4, [38]) to extract the temporal variance (( \sigma{t1}^2 ), ( \sigma{t2}^2 )) and the mean residence time (( t{01} ), ( t{02} )) for each window.
- Calculate Dispersion Coefficient: Using the two-window solution, compute the dispersion coefficient ( k ): ( k = \frac{u^2 (\sigma{t2}^2 - \sigma{t1}^2)}{2 (t{02} - t{01})} ) where ( u ) is the mean fluid speed.
- Calculate Diffusion Coefficient: Determine the diffusion coefficient using the capillary radius and the dispersion coefficient. For conditions where axial diffusion is negligible: ( D = \frac{Rc^2 u^2}{24k} ) For a more general solution (Taylor-Aris dispersion), use: ( D = \frac{1}{2} \left( \frac{Rc^2 u^2}{12k} + \sqrt{\left( \frac{Rc^2 u^2}{12k} \right)^2 + \frac{4Da^2}{3} } \right) ) where ( D_a ) represents the contribution of axial diffusion, often simplified to the equation found in [42].
- Calculate Hydrodynamic Radius: Use the Stokes-Einstein equation: ( Rh = \frac{kB T}{6 \pi \eta D} ) where ( k_B ) is Boltzmann's constant, ( T ) is temperature, and ( \eta ) is solvent viscosity.
Protocol: Single-Run Determination of the Diffusion Interaction Parameter (kD)
This advanced protocol allows for the determination of the concentration-dependent diffusion interaction parameter, kD, from a single experiment by analyzing the shape of the dispersion front [43].
- Preparation: Prepare a sufficiently concentrated sample solution.
- Injection and Dispersion: Inject a larger sample slug than used in the standard protocol. As it flows through the capillary, the slug will develop a dispersed front and rear interface.
- Profile Analysis: Measure the concentration profile (e.g., by UV absorbance) along the entire dispersed slug. The concentration varies from zero (pure buffer) to the maximum (injected concentration, C0).
- Data Processing: The dispersion coefficient ( k ) becomes a function of concentration, ( k(C) ). The analysis involves relating the shape of the concentration gradient at the front to the concentration dependence of the diffusion coefficient.
- Parameter Extraction: By fitting the resulting data to the appropriate model, the diffusion interaction parameter kD, which describes the nature and strength of molecular interactions (e.g., attractive or repulsive), can be extracted in a single run.
Quantitative Data and Validity Conditions
The following tables summarize the key validity conditions for TDA experiments and typical parameters for common analytes.
Table 1: Validity Conditions for TDA Experiments [38] [39]
| Condition | Mathematical Criterion | Practical Implication | Consequence of Violation |
|---|---|---|---|
| Radial Equilibrium | ( t0 > 1.7 \frac{Rc^2}{D} ) | Ensure flow is slow enough or capillary is long enough for solute to diffuse across the radius. | Systematic error in calculated D; peak shape may not be Gaussian. |
| Negligible Axial Diffusion | ( \text{Pe} = \frac{2 U R_c}{D} > 28.7 ) | Ensure flow is fast enough so that Taylor dispersion dominates over longitudinal diffusion. | Systematic error in calculated D. The full Taylor-Aris equation must be used. |
Table 2: Typical Parameters and Calculated Values for Common Analytes
| Analyte | Approx. Hydrodynamic Radius (Rh) | Diffusion Coefficient, D (m²/s) | Typical Capillary Radius (Rc) | Minimum Residence Time (t₀) |
|---|---|---|---|---|
| Small Molecule | 0.5 nm | ~5 × 10â»Â¹â° | 75 µm | > 4 seconds |
| Protein (BSA) | 3.5 nm | ~7 × 10â»Â¹Â¹ | 75 µm | ~ 23 seconds |
| Large Polymer | 50 nm | ~5 × 10â»Â¹Â² | 75 µm | ~ 5 minutes |
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for TDA
| Item | Function / Role in Experiment |
|---|---|
| Fused-Silica Capillary | The core component where Taylor dispersion occurs. Typical internal diameters are 75-150 µm. Its length and radius are critical parameters [38] [39]. |
| Run Buffer | The carrier solvent that establishes the baseline and drives the flow. It must be compatible with the sample and detection method. Filtered and degassed buffers are recommended [38]. |
| Standard Samples | Monodisperse molecules with known hydrodynamic radii (e.g., sucrose, bovine serum albumin) used for method validation and system qualification [43]. |
| Viscosity Standard | A solvent of known viscosity (e.g., pure water) at a controlled temperature, required for the accurate conversion of D to Rh via the Stokes-Einstein equation [38]. |
| 2',5,6',7-Tetraacetoxyflavanone | 2',5,6',7-Tetraacetoxyflavanone, CAS:80604-17-7, MF:C23H20O10, MW:456.4 g/mol |
| Diethyl (6-bromohexyl)phosphonate | Diethyl (6-bromohexyl)phosphonate, MF:C10H22BrO3P, MW:301.16 g/mol |
Fundamental Principles & Experimental Setup
Frequently Asked Questions (FAQs)
Q1: What is the core principle behind using ATR-FTIR to measure diffusion? ATR-FTIR spectroscopy measures diffusion by monitoring the time-dependent increase in the infrared absorption signal of a diffusant (e.g., a drug molecule) as it penetrates a biological matrix that is in intimate contact with the ATR crystal. The evanescent wave, which penetrates a few micrometers into the sample, probes the concentration of the diffusant at the crystal-sample interface. By tracking the absorption over time, one can quantify the diffusion process. [44] [45]
Q2: Why is ATR-FTIR particularly suitable for studying biological matrices? ATR-FTIR is a label-free, non-destructive technique that requires minimal sample preparation. It allows for the real-time monitoring of diffusion processes in hydrated, complex biological samples like gels, tissues, or hydrogels without the need for slicing or extensive processing, thereby preserving the sample's native state. [46] [44]
Q3: How do I select the right ATR crystal for my biological experiment? The choice of crystal depends on your sample's properties and experimental goals. Key considerations include chemical compatibility (to avoid reaction with the biological matrix), refractive index (must be higher than the sample), and the required wavelength range. Diamond is often preferred for its durability and broad spectral range, while germanium offers a higher refractive index for shallower penetration depth when analyzing surface domains. [44]
Research Reagent Solutions: Essential Materials for ATR-FTIR Diffusion Studies
The following table details key materials and their functions for successful experiment setup.
| Item | Function & Rationale |
|---|---|
| Diamond ATR Crystal | A robust, chemically inert crystal ideal for analyzing a wide range of biological samples, including hydrated materials; it provides a broad IR transmission range. [44] |
| Polymer Films / Biological Matrices | The model membrane or tissue being studied (e.g., glycerogelatin films, skin models). Its thickness and composition must be carefully controlled and documented for accurate diffusion modeling. [47] |
| Solvent/Diffusant with Distinct IR Peak | The drug solution or solvent whose diffusion is being tracked. It must possess a strong, distinctive absorption band (e.g., O-H stretch of water at ~3400 cmâ»Â¹) that does not overlap significantly with the matrix's peaks. [45] |
| Normalization Reference (Polymer Peak) | A stable absorption peak inherent to the biological matrix itself. This peak is used to normalize the diffusant's signal, accounting for potential physical changes in the film, such as swelling, during the experiment. [45] |
| Flow Cell or Sealed Chamber | An accessory that holds the ATR crystal and sample, allowing for controlled introduction of the diffusant and maintaining constant environmental conditions (e.g., temperature, humidity) throughout the experiment. [46] |
Measurement Protocols & Data Acquisition
Step-by-Step Experimental Workflow
The following diagram illustrates the core workflow for an ATR-FTIR diffusion experiment.
Detailed Protocol:
- Film Preparation & Mounting: Prepare a uniform film of your biological matrix (e.g., a polymer or tissue section). Carefully place it on the clean ATR crystal, applying consistent pressure to ensure optimal, void-free contact. [45]
- Collect Initial Reference Spectrum: Record the FTIR spectrum of the dry biological matrix alone. This serves as the initial background or reference state. [45]
- Introduce Diffusant: Apply the drug solution or solvent to the surface of the biological matrix opposite the ATR crystal. Ensure the application is consistent and does not disturb the film-crystal contact.
- Acquire Time-Series Spectra: Program the FTIR spectrometer to automatically collect spectra at defined, regular time intervals immediately after introducing the diffusant. Continue until the signal at the characteristic peak reaches a plateau, indicating equilibrium. [45] [48]
- Pre-process Spectral Data:
- Normalization: Use a dedicated, stable peak from the biological matrix (e.g., a C-H stretch) as an internal reference to normalize the diffusant's peak absorbance. This corrects for any swelling or physical changes in the film. [45]
- Spectral Difference: For enhanced sensitivity, subtract the initial reference spectrum (Step 2) from all subsequent time-series spectra. This technique effectively nulls the polymer signal, making positive bands from the diffusant more pronounced. [45]
- Model Fitting & Calculate D: The normalized absorbance data is fitted to a solution of Fick's second law, modified for the ATR geometry, to extract the diffusion coefficient (D). [48]
Quantitative Data from Literature
The table below summarizes diffusion coefficients measured via ATR-FTIR in various systems, providing a reference for expected values and experimental contexts.
| Diffusant | Matrix | Diffusion Coefficient (D) | Experimental Conditions & Notes |
|---|---|---|---|
| Ethanol-d | Glycerogelatin Film | Excellent reproducibility reported [47] | Measurement showed good agreement with traditional diffusion cell methods. [47] |
| Pyrolytic Oil | Aged Asphalt Binder | 10â»Â¹Â² to 10â»Â¹Â¹ m²/s [48] | Operando FTIR-ATR with Fickian model fitting; values comparable to commercial rejuvenators. [48] |
| Water | Polyethylene Terephthalate (PET) | ~10â»â¹ cm²/s (example for typical polymer) [45] | Measurement feasible due to strong/distinctive water peak at 3400 cmâ»Â¹, despite low equilibrium concentration. [45] |
Troubleshooting Common Experimental Issues
Frequently Asked Questions (FAQs)
Q4: My spectra show negative absorbance peaks. What is the cause? Negative peaks typically indicate that the ATR crystal was contaminated when the background reference spectrum was collected. Solution: Clean the ATR crystal thoroughly with an appropriate solvent, collect a new background spectrum, and then re-measure your sample. [49] [50]
Q5: I am getting noisy spectra with strange spectral features. How can I fix this? Noise and strange features are often caused by physical vibrations interfering with the highly sensitive interferometer in the FTIR. Solution: Ensure the instrument is placed on a stable, vibration-free bench. Move away potential sources of vibration, such as pumps, chillers, or heavy foot traffic. [49] [50]
Q6: My diffusion data does not fit the Fickian model well. What could be wrong? Non-ideal fitting can arise from several issues:
- Poor Film Contact: Inconsistent or poor contact between the biological matrix and the ATR crystal will distort the signal.
- Sample Swelling: Significant swelling of the matrix during diffusion can lead to non-Fickian behavior and poor model fitting. [45]
- Molecular Interactions: Specific interactions (e.g., hydrogen bonding) between the diffusant and the matrix can hinder diffusion and deviate from ideal Fickian behavior. [48]
Q7: The signal from my diffusant is very weak. What can I do to improve it?
- Use a Distinctive Peak: Ensure you are monitoring a strong, characteristic peak of the diffusant that does not overlap with matrix peaks. [45]
- Spectral Difference: Apply the spectral difference technique to enhance the visibility of the diffusant's peaks. [45]
- Horizontal ATR: Consider using a horizontal ATR setup, which can sometimes enhance the signal for certain sample types. [45]
Data Analysis, Error Estimation & Statistical Framework
Data Processing and Modeling Workflow
The logical flow for analyzing spectral data to obtain a statistically robust diffusion coefficient is outlined below.
Key Steps for Error Estimation and Analysis:
- Data Pre-processing: Always normalize the diffusant's peak intensity to an internal standard peak from the biological matrix to account for swelling and improve data quality for fitting. [45]
- Model Fitting: Use non-linear regression to fit the normalized time-absorption data to the appropriate solution of Fick's second law for the ATR geometry. The output is the diffusion coefficient (D). [48]
- Uncertainty Quantification: The curve-fitting algorithm should provide confidence intervals or standard errors for the estimated parameter (D). Reporting this is crucial for error estimation in your research. [45]
- Advanced Statistical Validation: For complex systems, especially those used in classification (e.g., diseased vs. healthy tissue), combine ATR-FTIR with multivariate statistical analysis:
- Principal Component Analysis (PCA): Can amplify subtle spectral differences related to the diffusion process or sample status. [51]
- Machine Learning Models: Linear Discriminant Analysis (LDA), Support Vector Machine (SVM), and k-Nearest Neighbor (kNN) can be built on spectral data to classify samples and validate findings with high accuracy. [51]
- Receiver Operating Characteristic (ROC) Analysis: Evaluates the performance of classification models, with an Area Under the Curve (AUC) >0.95 indicating excellent predictive ability. [51]
Troubleshooting Guide: Common Experimental Errors & Solutions
Q1: Our DTI tractography for neurosurgical planning shows inconsistent white matter pathways. What are the primary sources of error and how can we mitigate them?
A: Inconsistent tractography often stems from systematic errors and noise in DTI acquisition. These errors disrupt the accurate visualization of critical anatomical details necessary for clinical applications like neurosurgical planning [52].
Error Source 1: Systematic Spatial Errors
- Cause: Non-uniformity of magnetic field gradients, leading to inaccuracies in the B-matrix spatial distribution (BSD) [52].
- Solution: Implement B-matrix Spatial Distribution (BSD) correction. Phantom experiments show this correction has a substantially greater effect on improving DTI metric accuracy than denoising alone [52].
Error Source 2: Random Noise
- Cause: Inherent noise in MRI acquisition, which disrupts tensor calculation and tractography [52].
- Solution: Apply denoising algorithms as part of the preprocessing pipeline. The combined use of denoising and BSD correction has been shown to significantly improve Fractional Anisotropy (FA) and Mean Diffusivity (MD) measures, as well as overall tractography quality [52].
Error Source 3: Data Analysis Errors
- Cause: Applying incorrect preprocessing configurations or using a single correction method in isolation [52].
- Solution: Use a combined preprocessing pipeline. Research indicates that denoising and BSD correction are complementary steps and should be used together to reduce both random and systematic errors [52].
Q2: The ADC values from our oncology studies show poor repeatability, especially when using MR-Linac systems. How can we improve measurement consistency?
A: Poor ADC repeatability is a known challenge, particularly on MR-Linac systems, and is often related to geometric distortion and registration issues [53].
Error Source 1: Geometric Distortion
- Cause: Echo Planar Imaging (EPI)-based DWI sequences, which are highly susceptible to magnetic field inhomogeneities [53].
- Solution:
- Option A: Employ image registration of diffusion-weighted images to unweighted (b0) images. One study demonstrated this improved the repeatability coefficient (RC) in prostate gross tumor volume from 28.0% to 25.1% [53].
- Option B: Consider using low-distortion sequences like split acquisition of fast spin-echo signal (SPLICE). However, note that these may require further optimization as they can exhibit poorer repeatability compared to registered EPI [53].
Error Source 2: Region of Interest (ROI) Placement
Error Source 3: Model Selection
- Cause: Using a mono-exponential model for ADC calculation in tissues with complex microstructure where non-Gaussian effects are significant, particularly at high b-values (>1000 s/mm²) [54].
- Solution: For advanced applications, explore non-Gaussian diffusion models like Diffusion Kurtosis Imaging (DKI) or bi-exponential intravoxel incoherent motion (IVIM) to better capture tissue complexity [54].
Q3: When using ADC as a biomarker for treatment response, what statistical and cognitive errors should we be aware of in analysis?
A: Errors in interpreting quantitative imaging biomarkers like ADC span statistical, cognitive, and decision-making domains [55].
Error Source 1: Misinterpretation of Quantitative Results
- Cause: Confusing statistical "error" with biological "variability." Variability refers to differences in interpretation between observers or inherent biological heterogeneity, while error implies a deviation from a known ground truth [55].
- Solution: Clearly distinguish between variability (measured by inter-observer agreement indices) and true error in your analysis and reporting [55].
Error Source 2: Cognitive Bias in Decision-Making
- Cause: The radiological decision process is influenced by a priori probability (prior knowledge and context) and the decision criterion set by the physician. In oncology, a physician may be torn between a conservative objective (minimizing false positives) and a non-conservative objective (minimizing false negatives), which alters the decision threshold [55].
- Solution: Be explicit about the clinical context and decision goals. Use standardized reporting systems (e.g., BIRADS, RECIST) to frame the analysis task and minimize ad-hoc decision thresholds [55].
Error Source 3: Over-reliance on Single Time Points
- Cause: Assessing treatment response based on ADC at a single time point may miss the dynamic nature of response [56].
- Solution: Implement serial imaging and advanced analysis like Functional Diffusion Mapping (FDM), which quantifies the percentage of voxels with significantly changed ADC. For Head & Neck SCC, week 3 during radiotherapy was identified as the optimal time point for outcome prediction using FDM metrics [56].
Quantitative Reference Tables for ADC and DTI in Oncology
Table 1: Pooled Correlation between ADC and Tumor Cellularity by Cancer Type (Meta-Analysis Data)
| Tumor Type | Pooled Correlation Coefficient (Ï) | 95% Confidence Interval | Strength of Correlation |
|---|---|---|---|
| Glioma | -0.66 | [-0.85; -0.47] | Strong |
| Ovarian Cancer | -0.64 | [-0.76; -0.52] | Strong |
| Lung Cancer | -0.63 | [-0.78; -0.48] | Strong |
| Uterine Cervical Cancer | -0.57 | [-0.80; -0.34] | Moderate |
| Prostatic Cancer | -0.56 | [-0.69; -0.42] | Moderate |
| Renal Cell Carcinoma | -0.53 | [-0.93; -0.13] | Moderate |
| Head and Neck SCC | -0.53 | [-0.74; -0.32] | Moderate |
| Breast Cancer | -0.48 | [-0.74; -0.23] | Weak-to-Moderate |
| Meningioma | -0.45 | [-0.73; -0.17] | Weak-to-Moderate |
| Lymphoma | -0.25 | [-0.63; 0.12] | Weak/Not Significant |
Data derived from a meta-analysis of 39 publications with 1530 patients [57].
Table 2: Advanced ADC Metrics for Differentiating Breast Lesions (Diagnostic Performance)
| ADC Metric | Description | Diagnostic Utility |
|---|---|---|
| ADC_min | Minimum ADC value within a tumor, capturing areas of highest cell density and most restricted diffusion [58]. | Most effective single indicator for differentiating benign and malignant breast tumors [58]. |
| ADC_avg (or Mean ADC) | The average apparent diffusion coefficient across the region of interest based on a mono-exponential model [58] [54]. | Commonly used but may oversimplify tumor heterogeneity; improved diagnostic performance when combined with other metrics [58]. |
| rADC_min | Relative ADC ratio (lesion ADC_min / ADC of a reference tissue such as normal glandular tissue, pectoralis muscle, or interventricular septum) [58]. | Standardizes the lesion's ADC, minimizing bias from inter-individual tissue variability and improving diagnostic stability [58]. |
| ADC_cv | Coefficient of variation (standard deviation/mean) of ADC measurements within a lesion [58]. | Reflects the heterogeneity of diffusion within the tumor, which can be a marker of malignancy [58]. |
Data supporting the use of advanced ADC metrics is based on a retrospective cohort analysis of 125 pathologically confirmed breast tumors [58].
Essential Experimental Protocols
Protocol 1: DTI for Neurosurgical Planning and Tractography
This protocol is critical for preoperative mapping of eloquent white matter tracts to maximize tumor resection while preserving functional tissue [59].
- Objective: To preoperatively map functionally relevant white matter tracts (WMT) and assess their relationship with brain tumors to reduce postoperative deficits [59].
- Key Applications:
- Defining tumor proximity to WMT and assessing tumor impact (displacement, invasion, or destruction) [59].
- Selecting the optimal surgical approach by comparing how potential access routes impact WMT [59].
- Aiding in the selection of patients for resective surgery, particularly those with tumors embedded in or near eloquent regions [59].
- Methodology:
- Data Acquisition: Acquire DTI data using a single-shot EPI sequence. The use of parallel imaging (e.g., ASSET) can reduce distortion. Diffusion gradients are typically applied in multiple directions (e.g., 6-32) with at least two b-values (e.g., b=0 and b=600-1000 s/mm²) [59] [60].
- Preprocessing: Implement a combined preprocessing pipeline including denoising and B-matrix Spatial Distribution (BSD) correction to significantly reduce random and systematic errors, thereby improving the accuracy of FA and MD measures [52].
- Tractography: Generate DTI-derived tractography (DDT) to visualize white matter pathways. Use deterministic or probabilistic algorithms to reconstruct tracts of interest (e.g., corticospinal tract, arcuate fasciculus). Altered WMT position (displacement) or decreased WMT density can indicate tumor invasion or edema [59].
- Troubleshooting Note: DTI and DDT are primarily used adjunctively with techniques like direct electrical stimulation (DES). They help in planning DES sites but are not yet a complete substitute [59].
Protocol 2: Quantitative ADC for Differentiating Breast Ductal Carcinoma In Situ (DCIS) from Invasive Breast Carcinoma (IBC)
This protocol uses DTI metrics as an adjunct to Dynamic Contrast-Enhanced MRI (DCE-MRI) to improve diagnostic accuracy [60] [61].
- Objective: To improve the accuracy of differential diagnosis between DCIS and IBC by combining quantitative DTI measurements with conventional DCE-MRI [60].
- Key Findings: A multivariate model identified the Exponential Attenuation (EA) value from DTI, lesion enhancement style, and Time-Intensity Curve (TIC) pattern as independent factors for differential diagnosis. The combination showed higher diagnostic efficacy than DCE-MRI alone (AUC improved from 0.84 to 0.94) [60] [61].
- Methodology:
- MRI Acquisition: Perform DCE-MRI, DWI, and DTI on a 1.5T or 3T scanner using a dedicated breast coil. For DTI, use a single-shot EPI sequence with diffusion gradients applied in at least 6 directions and b-values of 0 and 600 s/mm² [60].
- ROI Placement: Manually draw Regions of Interest (ROIs) on the largest solid area of the lesion, carefully excluding cystic changes, hemorrhage, necrosis, and fat. ROIs should be placed on parameter maps (ADC, FA, etc.) cross-referenced with enhanced MRI for accurate localization [60].
- Parameter Calculation: Extract multiple quantitative parameters:
- From DWI: Apparent Diffusion Coefficient (ADC).
- From DTI: Directionally-averaged mean diffusivity (Davg), Exponential Attenuation (EA), Fractional Anisotropy (FA), Relative Anisotropy (RA), and Volume Ratio (VR) [60].
- Statistical Analysis: Use multivariate logistic regression to identify independent predictors. Evaluate diagnostic performance using Receiver Operating Characteristic (ROC) curve analysis [60].
Visualization: Error Mitigation Workflow in DTI
The following diagram illustrates a recommended workflow to mitigate systematic and random errors in DTI processing, which is critical for obtaining reliable data for clinical and research applications.
Diagram Title: DTI Preprocessing for Error Reduction
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Analytical Tools for DTI/ADC Research
| Item / Solution | Function / Application in Research |
|---|---|
| 1.5T or 3T MRI Scanner with High-Performance Gradients | Essential hardware for acquiring DWI and DTI data. Higher field strengths and advanced gradients enable more advanced diffusion modeling (e.g., for non-Gaussian diffusion) and reduce distortion [54]. |
| Dedicated Coils (e.g., Breast, Neurovascular) | Specialized radiofrequency coils designed for specific body parts are crucial for achieving a high signal-to-noise ratio (SNR) in the region of interest [60] [58]. |
| Phantom for Diffusion MRI | A standardized object with known diffusion properties used for quality control, calibration, and validation of ADC and DTI metrics. Critical for assessing and correcting systematic errors [52] [53]. |
| Post-Processing Software with Denoising & BSD Correction | Software tools that implement algorithms for denoising and B-matrix Spatial Distribution (BSD) correction are necessary to reduce both random and systematic errors, significantly improving the accuracy of FA, MD, and tractography [52]. |
| Image Registration Software | Software capable of aligning different MRI sequences (e.g., DWI to T1-weighted) or serial scans. This improves the repeatability of ADC measurements, especially in longitudinal treatment response studies [53]. |
| Bi-exponential / IVIM and Kurtosis Modeling Software | Advanced analytical tools that move beyond the mono-exponential ADC model. They are used to separate effects of microcirculation (IVIM) and tissue complexity (DKI), providing more specific microstructural information [54]. |
| Thiophene-2-amidoxime | N-Hydroxythiophene-2-carboximidamide|CAS 53370-51-7 |
Pitfalls and Solutions: Optimizing Accuracy in Diffusion Analysis
Conceptual Foundation: SD vs. SE
In statistical analysis, particularly in diffusion coefficient research, distinguishing between standard deviation (SD) and standard error (SE) is fundamental for accurate data interpretation and reporting.
- Standard Deviation (SD): This measures the variability or spread of individual data points around the sample mean. It describes the dispersion of your raw data. A large SD indicates high variability among individual observations, while a small SD suggests data points are clustered closely around the mean [62] [63] [64]. SD is a descriptive statistic.
- Standard Error (SE), specifically the Standard Error of the Mean (SEM): This measures the precision of your sample mean as an estimate of the true population mean. It estimates how much the sample mean would vary if you were to repeat the entire sampling process multiple times. SE is an inferential statistic [62] [63] [65].
The core relationship is given by the formula:
SE = SD / √n
where n is the sample size [62] [66] [63]. This formula highlights a critical distinction: while SD is largely unaffected by sample size, SE decreases as sample size increases [67] [64]. This reflects the principle that larger samples provide more precise estimates of the population mean.
Comparative Analysis: Key Differences
The table below summarizes the core distinctions between Standard Deviation and Standard Error.
Table 1: Standard Deviation vs. Standard Error
| Aspect | Standard Deviation (SD) | Standard Error (SE) |
|---|---|---|
| Measures | Variability of individual data points [68] [63] | Precision of the sample mean estimate [68] [63] |
| What it Describes | Spread of the data [64] | Uncertainty in the mean [64] |
| Use Case | Descriptive statistics; understanding data dispersion [62] [67] | Inferential statistics; confidence intervals, hypothesis testing [62] [67] |
| Impact of Sample Size | No predictable change with increasing n [67] [63] |
Decreases as sample size (n) increases [62] [67] [64] |
| Formula | s = √[ Σ(xi - x̄)² / (n-1) ] |
SE = s / √n [62] [66] |
Troubleshooting Guide: FAQs and Solutions
This section addresses common pitfalls and questions researchers face when applying these concepts.
FAQ 1: I used error bars in my graph, but my colleague asked if they show SD or SE. How do I decide which to use?
- Solution: The choice depends on your graphical communication goal.
- Use SD error bars when you want to show the natural variability of the raw data itself among individuals in your sample. This allows readers to see the spread of the observations [67].
- Use SE error bars when you want to show the precision of your estimated means and how precisely the sample mean represents the population mean. This is often used to give a visual impression for statistical significance between groups; if the 2*SE error bars of two means do not overlap, it suggests a significant difference [65].
- Critical Action: Always label your error bars clearly in the figure legend as "±SD" or "±SE" to avoid misinterpretation [68] [63].
FAQ 2: My mean diffusion coefficient is 5.2 µm²/s. Should I report ±SD or ±SE with this value in my paper?
- Solution: This is a frequent point of confusion in scientific literature.
- Report the Standard Deviation (±SD) when your goal is to describe your sample. It gives context about the heterogeneity of the measurements you observed. For example: "The measured diffusion coefficient was 5.2 ± 1.8 µm²/s (mean ± SD)." This tells the reader the typical deviation of individual molecule measurements from the mean [67] [65].
- Report the Standard Error (±SE) when your goal is to make an inference about the population mean from your sample data, especially when constructing confidence intervals. For example: "The estimated population diffusion coefficient was 5.2 ± 0.4 µm²/s (mean ± SE)." This communicates the uncertainty of your estimate [67].
FAQ 3: I calculated a very small Standard Error. Does this mean the variability in my data is low?
- Solution: Not necessarily. A small SE primarily indicates that your sample mean is a precise estimate of the population mean, which is heavily influenced by a large sample size. Your data could still have very high variability (a large SD), but by measuring a large number of observations (
n), you have zeroed in on the population mean with high precision [68]. Always check the SD to understand the underlying variability of your data.
FAQ 4: Are the terms "Standard Error" and "Standard Error of the Mean (SEM)" interchangeable?
- Solution: While "Standard Error of the Mean (SEM)" is the most common and specific term, "Standard Error (SE)" is widely used to refer to the same concept. However, technically, standard errors can be calculated for other statistics (like a proportion or a regression coefficient). In the context of means, they are generally considered synonymous [66] [69].
Experimental Protocol for Error Estimation
This section provides a step-by-step methodology for calculating and applying SD and SE in a typical analysis, such as estimating a diffusion coefficient from experimental data.
Table 2: Research Reagent Solutions for Data Analysis
| Item | Function in Analysis |
|---|---|
| Statistical Software (e.g., R, Python, Prism) | Performs complex calculations of SD, SE, and other statistics; generates plots and error bars. |
| Dataset | The raw experimental measurements (e.g., particle trajectories, intensity fluctuations). |
| Computational Formula for SD | Provides the algorithm for calculating sample standard deviation. |
| Sample Size (n) | The number of independent observations or replicates, critical for calculating SE. |
Step-by-Step Workflow:
- Data Collection: Perform your experiment (e.g., single-particle tracking) and record all raw measurements. Ensure an adequate sample size (
n) for reliable inference. - Calculate Sample Mean (x̄): Sum all observations and divide by the number of observations (
n). - Calculate Sample Standard Deviation (SD):
a. Find the difference between each observation and the mean (
xi - x̄). b. Square each difference ((xi - x̄)²). c. Sum all the squared differences (Σ(xi - x̄)²). d. Divide this sum byn-1(to get the sample variance). e. Take the square root of the result to obtain the SD [68] [70]. - Calculate Standard Error of the Mean (SE): Divide the calculated SD by the square root of your sample size:
SE = SD / √n[62] [69]. - Reporting:
The following diagram illustrates the logical decision process for applying SD and SE in data analysis.
Overcoming Sub-diffusive Dynamics in MD Simulations to Prevent Overestimation
FAQs: Understanding Sub-Diffusion and Overestimation
What is sub-diffusive dynamics and why does it occur in MD simulations?
Subdiffusion is a type of anomalous diffusion where the Mean Squared Displacement (MSD) of a particle increases with time according to a power law, MSD ∠Dαtα, with 0 < α < 1, rather than the linear relationship (MSD ∠Dt) characteristic of normal, Brownian diffusion [71]. In molecular dynamics (MD) simulations, this behavior is often observed transiently before a crossover to standard Brownian dynamics [71]. It is a common phenomenon in viscoelastic and crowded environments like lipid bilayers or polymeric materials, where persistent correlations and memory effects in particle-environment interactions hinder molecular motion [71] [72] [73]. If a simulation is not run long enough for the system to transition from this subdiffusive regime to the normal diffusive regime, the calculated diffusion coefficients can be dramatically over-predicted [73].
What are the key indicators that my simulation is affected by sub-diffusive dynamics?
The primary indicator is a non-linear, power-law increase in the MSD when plotted against time on a log-log scale [71] [72]. You should calculate the MSD for your molecule of interest and analyze its behavior.
- MSD Analysis: For simple diffusion, the MSD increases linearly with time. A plot of MSD vs. time that is concave downward suggests confined or corralled motion, which can manifest as subdiffusion [74].
- Crossover Time: The transition from subdiffusive to normal Brownian dynamics occurs over a characteristic crossover time. This timescale can vary greatly, from nanoseconds in simple, uncrowded systems to arbitrarily long times in crowded environments [71]. Your simulation must significantly exceed this crossover time to yield accurate diffusion coefficients [73].
What is the concrete risk of not accounting for sub-diffusion?
The principal risk is a dramatic over-prediction of the diffusion coefficient, D [73]. When diffusion coefficients are calculated from data that is still within the subdiffusive regime, the values are not physically meaningful for long-timescale transport properties like membrane permeability [72]. This can lead to fundamentally incorrect conclusions about the system's behavior, such as overestimating the permeability of a drug molecule through a membrane or the leaching rate of a compound from a polymer [73].
Are certain types of systems more prone to this problem?
Yes. Systems with inherent crowding, heterogeneity, and viscoelasticity are particularly susceptible. Key examples from research include:
- Proteins and lipids in biological membranes: The densely packed, heterogeneous structure of membranes naturally leads to subdiffusive behavior on nanosecond timescales [71] [72].
- Ion transport in solids: Simulations of solid-state ionics must confirm the transition from subdiffusive to diffusive behavior for reliable results [75].
- Small molecules in polymers: Drug-like molecules diffusing through polymeric matrices used in medical devices exhibit prolonged subdiffusive dynamics [73].
Troubleshooting Guides
Guide 1: Diagnosing Sub-Diffusive Dynamics in Your Simulation
This protocol outlines the steps to analyze your MD trajectory and determine if subdiffusion is affecting your results.
Step 1: Calculate the Mean Squared Displacement (MSD)
- Methodology: From your production trajectory, extract the positions of the molecule(s) of interest over time. For a set of time lags (Δt), compute the MSD. For three-dimensional diffusion, the MSD is generally calculated as MSD(Δt) = ⟨ |r(t + Δt) - r(t)|² ⟩, where r(t) is the position vector at time t and the angle brackets denote an average over all time origins, t [74] [4].
- Protocol Tip: Ensure your trajectory is long enough to observe the onset of linear MSD behavior. Using overlapping time windows in your calculation improves statistics, but be aware that this introduces correlations that complicate error estimation [74].
Step 2: Plot and Fit the MSD Curve
- Methodology: Plot the MSD as a function of the time lag, Δt, on a log-log scale. Also, create a linear-scale plot. On the log-log plot, a straight line suggests a power-law relationship (MSD ∠tα). The slope of this line is the anomalous exponent α. On the linear plot, a straight line indicates normal diffusion (α=1) [74].
- Protocol Tip: The MSD for true simple diffusion on a linear scale has a slope of 2dD, where d is the dimensionality of your data (e.g., d=2 for two dimensions) [74].
Step 3: Identify the Dynamical Regime and Crossover
- Methodology: Analyze the MSD plots to identify the different dynamical regimes.
- Protocol Tip: The crossover time from subdiffusive to Brownian dynamics is the critical timescale your simulation must exceed [71].
The logical workflow for this diagnostic process is outlined below.
Guide 2: Preventing Overestimation of Diffusion Coefficients
This guide provides strategies to ensure your simulations produce accurate, reliable diffusion coefficients.
Strategy 1: Ensure Adequate Simulation Length
- Action: The simulation duration must be significantly longer than the characteristic crossover time from subdiffusive to normal diffusion [73]. For new systems, run preliminary tests to estimate this crossover time.
- Technical Note: In crowded membranes or dense polymers, this crossover can take hundreds of nanoseconds or even microseconds [71] [73]. Do not calculate the diffusion coefficient until the MSD shows a clear linear regime.
Strategy 2: Employ Robust Analysis Methods
- Action: Consider using Maximum Likelihood-based Estimation (MLE) as an alternative to standard MSD analysis for calculating diffusion coefficients.
- Technical Note: MSD analysis from single trajectories has statistical shortcomings, including an asymmetric distribution of estimated D values and difficulty handling localization uncertainty. MLE has been shown to provide superior performance, especially for trajectories with large localization errors or slow movements [4].
Strategy 3: Apply a Generalized Theoretical Framework
- Action: For systems where subdiffusion is intrinsic, model the dynamics with a Generalized Langevin Equation (GLE) that incorporates memory effects.
- Technical Note: GLE models use a memory kernel to account for time-dependent friction. Models based on Mittag-Leffler-type memory kernels can naturally reproduce the ballistic, subdiffusive, and Brownian regimes, as well as the crossovers between them, providing a more consistent picture of diffusion [71].
Strategy 4: Pre-Simulation Checks
- Action: Before starting a production run, double-check critical simulation parameters to avoid wasting computational resources [25].
- Technical Note: Verify that temperature and pressure coupling parameters match your equilibration steps. Use auto-fill features for input paths to prevent errors, and save your configuration for reproducibility [25].
The following diagram summarizes the key steps for a reliable simulation workflow.
The Scientist's Toolkit
Research Reagent Solutions
This table details key materials and computational tools referenced in the troubleshooting guides.
| Item/Reagent | Function/Explanation | Example Context |
|---|---|---|
| Generalized Langevin Equation (GLE) Model | A theoretical framework that incorporates memory effects via a "memory kernel" to describe non-Markovian dynamics and crossover from subdiffusive to Brownian motion [71]. | Modeling protein lateral diffusion in lipid membranes [71]. |
| Mittag-Leffler Function | A multi-parameter function used to model the elastic (non-instantaneous) component of the memory kernel in viscoelastic GLE models [71]. | Describing the time-dependent membrane response in constitutive equations [71]. |
| Maximum Likelihood Estimation (MLE) | A robust statistical method for estimating diffusion coefficients from single-particle trajectories. It outperforms MSD analysis when dealing with localization errors or short trajectories [4]. | Analyzing receptor dynamics in live-cell single-molecule tracking [4]. |
| NIST-Traceable Diffusion Phantom | A physical reference standard with known diffusion coefficients used to validate and control the quantitative accuracy of diffusion measurements in MRI systems [76]. | Quality assurance for ADC measurements across multiple MRI scanners [76]. |
| Adaptive Biasing Force (ABF) Algorithm | An enhanced sampling method used to calculate the free-energy profile (Potential of Mean Force) for a molecule crossing a membrane [72]. | Determining the free-energy barrier for methanol permeation through a POPC bilayer [72]. |
Table 1: Characteristic Dynamical Regimes in Molecular Diffusion
This table summarizes the different dynamical regimes and their MSD signatures, as observed in MD simulations.
| Dynamical Regime | MSD Proportionality | Typical Timescale | Physical Origin |
|---|---|---|---|
| Ballistic | t² | < 100 fs [72] | Particle inertia, free streaming before collisions. |
| Subdiffusive | tα (0<α<1) | Transient, from ~100 fs to >10 ns (up to seconds in complex systems) [71] [72] | Crowding, viscoelasticity, trapping, and persistent correlations. |
| Brownian (Normal) | t | Long times, exceeding the system's characteristic crossover time [71] | Classical random walk, where numerous collisions lead to a linear MSD. |
Table 2: Comparison of Diffusion Coefficient (D) Estimation Methods
This table compares the two primary methods for calculating diffusion coefficients from particle trajectories.
| Method | Key Principle | Advantages | Limitations / Best For |
|---|---|---|---|
| Mean Squared Displacement (MSD) | Fits the slope of the MSD vs. time curve. For normal diffusion in dimension d, MSD = 2dDt [74] [4]. | Intuitive, widely used, provides consistent results for long, well-behaved trajectories [4]. | Prone to complex noise and statistical bias from overlapping averages; poorly handles localization error [4]. |
| Maximum Likelihood Estimation (MLE) | Finds the parameter D that maximizes the probability of observing the given trajectory [4]. | More accurate, especially for short trajectories, large localization errors, or slow diffusion; handles motion blur [4]. | More complex implementation; requires a specific model of the diffusion process. |
In research focused on error estimation and statistical analysis, particularly in fields like drug development and diffusion coefficients research, selecting the appropriate regression model is paramount. Ordinary Least Squares (OLS) regression is a fundamental technique used to model the relationship between a dependent variable and one or more independent variables. It works by minimizing the sum of the squared differences between the observed and predicted values [77]. While OLS is a powerful and widely used tool, especially for linear regression models, understanding its limitations is crucial for scientists to avoid misinterpretations and to ensure the validity of their experimental conclusions. This guide provides troubleshooting advice and FAQs to help researchers navigate these challenges.
Troubleshooting Guides
Guide 1: Diagnosing and Addressing Common OLS Violations
Problem: You suspect that the core assumptions of your OLS model are not met, potentially biasing your results.
Background: The OLS procedure produces the best possible estimates only when its classical assumptions are satisfied [78]. Violations can lead to biased coefficients, incorrect standard errors, and unreliable hypothesis tests.
Steps:
- Check for Linearity: The relationship between the independent and dependent variables should be linear in the parameters. Create scatter plots of the dependent variable against each independent variable. If you see a clear curved pattern, the linearity assumption may be violated.
- Check for Normality of Errors: The error term should be normally distributed. This is important for conducting hypothesis tests and constructing confidence intervals. Use a Normal Probability Plot (Q-Q plot) of the residuals; points should roughly follow a straight line [78].
- Check for Homoscedasticity: The variance of the error term should be constant. Plot the residuals against the fitted (predicted) values. The spread of residuals should be random and not form patterns like a cone (increasing or decreasing spread) [78].
- Check for Autocorrelation: In time-series or sequentially collected data, error terms should not be correlated with each other. Plot residuals in the order of data collection and look for cyclical or trending patterns. The Durbin-Watson statistic is a formal test for this [78].
- Check for Multicollinearity: Independent variables should not be perfectly (or highly) correlated. Calculate the Variance Inflation Factor (VIF) for each variable. A VIF greater than 10 often indicates severe multicollinearity [78].
Resolution:
- Non-linearity: Consider transforming variables (e.g., log, square root) or using nonlinear regression models.
- Heteroscedasticity: Use robust standard errors, which provide more reliable inference even when variance is not constant.
- Autocorrelation: Consider adding relevant variables to the model or using time-series specific models (e.g., ARIMA).
- Multicollinearity: Remove or combine the highly correlated variables, or use regularization techniques like Ridge Regression.
Guide 2: Handling Outliers and Choosing Robust Alternatives
Problem: Your dataset contains outliers, which are exerting undue influence on the OLS model results.
Background: OLS minimizes the sum of squared errors. Because outliers have large errors, their influence is squared, making them disproportionately impactful and potentially pulling the regression line in their direction [77].
Steps:
- Identify Outliers: Create diagnostic plots such as:
- Residuals vs. Fitted Plot: Points far from zero may be outliers.
- Leverage Plots (Hat Values): Identify points with high leverage, meaning their x-values are unusual.
- Influence Plots (Cook's Distance): Identify points that have a strong influence on the regression model. A Cook's distance greater than 1 is often a cause for concern.
- Investigate Outliers: Determine if the outlier is a data entry error, a measurement error, or a valid but extreme data point. Never discard an outlier without a scientific justification.
- Assess Impact: Run the model with and without the outliers and compare the coefficient estimates and R-squared values. A significant change indicates high influence.
Resolution:
- If an outlier is a proven error, correct or remove it.
- If the outlier is valid, consider using a regression technique that is less sensitive to outliers. Least Absolute Deviations (LAD) Regression minimizes the sum of absolute errors instead of squared errors, giving outliers less weight [77].
- Transforming the dependent variable can sometimes reduce the impact of outliers.
Frequently Asked Questions (FAQs)
Q1: What is the core difference between linear regression and OLS? A: Linear regression is a broad class of statistical models that describe a linear relationship between variables. OLS is a specific optimization technique used within linear regression to find the best-fitting line by minimizing the sum of squared differences between observed and predicted values [77].
Q2: My model has high multicollinearity. What are my options? A: High multicollinearity occurs when independent variables are highly correlated, which inflates standard errors and makes coefficient estimates unstable [78]. Your options include:
- Remove one of the correlated variables if it is redundant.
- Combine the correlated variables into a single index (e.g., via Principal Component Analysis).
- Use regularization methods like Ridge or Lasso Regression, which penalize model complexity and can handle multicollinearity effectively.
Q3: When should I consider an alternative to OLS regression? A: You should consider an alternative when:
- Your data contains influential outliers [77].
- The relationship between variables is inherently non-linear.
- The variance of the errors is not constant (heteroscedasticity) and cannot be easily corrected.
- You are working with non-continuous data (e.g., binary outcomes, counts), which require Generalized Linear Models (GLMs).
- The goal is variable selection in a high-dimensional dataset, where Lasso Regression can be more effective.
Q4: How are diffusion coefficients used in reactor design, and what does this have to do with OLS? A: In chemical processes like glucose hydrogenation to produce sorbitol, diffusion coefficients are critical parameters for designing and simulating reactors. These coefficients are often determined experimentally, and regression models (which could be based on OLS) are used to analyze the data and model their relationship with factors like temperature and concentration. Using inaccurate models (like an OLS model that violates assumptions) to estimate these coefficients can lead to incorrect predictions of reactant conversion in the reactor, as shown in simulations where predicted glucose conversion profiles differed based on how diffusion coefficients were estimated [79].
Q5: What is the Gauss-Markov Theorem, and why is it important? A: The Gauss-Markov Theorem states that under the classical OLS assumptions (linearity, exogeneity, no autocorrelation, homoscedasticity, no perfect multicollinearity), the OLS estimators are the Best Linear Unbiased Estimators (BLUE). This means that among all linear unbiased estimators, OLS provides the estimates with the smallest variance, making them the most precise and reliable [77] [78].
Experimental Protocols & Data
Key Experimental Methodology: Determining Diffusion Coefficients
The accurate measurement of diffusion coefficients is a common task in physicochemical research where regression models are applied. The following protocol is adapted from studies on mass transfer in supercritical water systems [80].
Objective: To determine the self-diffusion coefficient of a solute (e.g., Hâ‚‚, CO, COâ‚‚, CHâ‚„) in a binary mixture with supercritical water (SCW) under confinement in carbon nanotubes (CNTs).
Materials:
- Simulation Software: Molecular Dynamics (MD) simulation package (e.g., GROMACS, LAMMPS).
- Force Field Models: SPC/E model for water molecules; Saito model for carbon nanotubes.
- Initial Configuration: A simulation box containing a CNT surrounded by SCW and solute molecules.
- Computational Cluster: High-performance computing resources for running nanosecond-scale simulations.
Procedure:
- System Setup: Construct the CNT of a specific diameter (e.g., 9.49 - 29.83 Ã…). Place it in the center of a simulation box and fill the interior and surrounding space with SCW and solute molecules at the desired molar concentration (e.g., 0.01 - 0.3).
- Energy Minimization: Run an energy minimization algorithm to remove any steric clashes or unrealistic geometries in the initial configuration.
- Equilibration: Perform an MD simulation in the NVT (constant Number, Volume, Temperature) ensemble followed by the NPT (constant Number, Pressure, Temperature) ensemble to bring the system to a state of thermodynamic equilibrium at the target conditions (e.g., 673-973 K, 25-28 MPa).
- Production Run: Execute a final, longer MD simulation to collect trajectory data. The mean squared displacement (MSD) of the solute molecules over time is calculated from this trajectory.
- Data Analysis: The self-diffusion coefficient (D) is calculated from the MSD data using the Einstein relation: ( D = \frac{1}{6N} \lim{t \to \infty} \frac{d}{dt} \sum{i=1}^{N} \langle |ri(t) - ri(0)|^2 \rangle ), where ( r_i(t) ) is the position of molecule i at time t, and N is the number of dimensions. For anomalous data, a machine learning clustering method can be employed to optimize the MSD-t data [80].
- Model Fitting: A mathematical model can be developed to predict the diffusion coefficients based on the simulation results. The goodness-of-fit of this model is often assessed using metrics like R², which can be derived from an OLS regression [80].
The table below summarizes key relationships observed in diffusion coefficient studies, which are often modeled using regression techniques.
Table 1: Factors Influencing Confined Self-Diffusion Coefficients in SCW Mixtures [80]
| Factor | Effect on Solute Diffusion Coefficient | Notes |
|---|---|---|
| Temperature | Increases linearly | Higher thermal energy enhances molecular motion. |
| CNT Diameter | Increases and then saturates | Confinement effect weakens as diameter increases beyond a certain point. |
| Solute Concentration | Remains relatively constant | Effect is minimal within the studied concentration range (0.01-0.3 molar). |
Research Reagent Solutions
Table 2: Essential Materials for Molecular Dynamics Studies of Diffusion [80]
| Item | Function in the Experiment |
|---|---|
| SPC/E Water Model | A classical force field model used to simulate the behavior and interactions of water molecules in the SCW state. |
| Saito CNT Model | A potential function used to describe the carbon-carbon interactions within the carbon nanotube, defining its rigid structure. |
| Molecular Dynamics (MD) Software | Software suite used to simulate the physical movements of atoms and molecules over time under specified conditions. |
| Machine Learning Clustering Algorithm | A computational method used to process and extract reliable diffusion coefficients from anomalous or noisy MSD-t data. |
Workflow and Relationship Diagrams
Diagram 1: OLS Diagnosis and Remediation Workflow
The diagram below outlines a logical workflow for diagnosing common OLS issues and selecting appropriate remedial actions.
Diagram 2: Relationship Between OLS Assumptions and Model Threats
This diagram visualizes the logical relationship between core OLS assumptions and the potential threats to model validity if they are violated.
Frequently Asked Questions
Q1: Why should I use Generalized Least Squares (GLS) instead of Ordinary Least Squares (OLS) for analyzing my Mean Squared Displacement (MSD) data?
Ordinary Least Squares (OLS) is statistically inefficient for MSD analysis and significantly underestimates the true uncertainty in the estimated diffusion coefficient because its core assumptions are violated. MSD data from molecular dynamics simulations or single-particle tracking is both serially correlated (MSD values at adjacent time intervals are similar) and heteroscedastic (the variance of MSD points is not constant) [3]. Using OLS under these conditions results in a relatively large statistical uncertainty for the diffusion coefficient, and the textbook formula for its uncertainty is misleadingly small, creating overconfidence in the results [3]. GLS, by explicitly incorporating the covariance structure of the data, provides the theoretical maximum statistical efficiency, meaning it gives the smallest possible uncertainty for the estimated parameter [3] [81].
Q2: How do I determine the covariance matrix (Σ) needed for a GLS analysis of my MSD data?
The true covariance matrix for a specific dataset is generally unknown. The established strategy is to approximate it using an analytical model covariance matrix, Σ′, which is parametrized from your observed simulation data [3]. This model is often derived for an equivalent system of freely diffusing particles. The "kinisi" Python package, referenced in the literature, implements such a method, using an analytical covariance matrix and Bayesian regression to sample compatible linear models [3]. For simpler cases, some studies suggest that a well-chosen number of MSD points in an unweighted fit can also yield a reliable estimate, but this depends on experimental parameters like the reduced localization error [29].
Q3: What is the "optimal number" of MSD points to use in the fitting procedure?
The optimal number of MSD points is not a fixed value but depends on your specific data. The key parameter is the reduced localization error, x = σ²/DΔt, where σ is the localization uncertainty, D is the diffusion coefficient, and Δt is the frame duration [29].
- When x ≪ 1 (negligible localization error), the best estimate is often obtained using just the first two MSD points [29].
- When x ≫ 1 (significant localization error), the standard deviation of the first few MSD points is dominated by this uncertainty, and a larger number of points, pmin, is needed for a reliable estimate. This optimal number pmin depends on both x and the total number of points N in the trajectory [29].
Q4: My GLS-fitted diffusion coefficient has high uncertainty. What are the main sources of this error?
High uncertainty can stem from several sources related to the data and the analysis:
- Insufficient trajectory length: Short trajectories provide limited sampling of the possible particle dynamics.
- Large localization uncertainty: This adds noise to each measured position, which propagates into the MSD calculation [29].
- Finite camera exposure time: During the exposure time, a fast-diffusing particle moves, blurring its position and effectively increasing the dynamic localization uncertainty [29].
- An imperfect covariance matrix model: If the model Σ′ does not accurately capture the true correlation structure of your data, the GLS efficiency will be reduced [3].
Troubleshooting Guides
Issue 1: Underestimated Uncertainty in Diffusion Coefficient
Problem: The confidence interval for my fitted diffusion coefficient from an OLS analysis is very small, but results are inconsistent between replicate simulations.
Diagnosis: This is a classic symptom of using an inappropriate regression method. OLS assumes no correlation between data points, which is false for MSD data. The analytical uncertainty from OLS is not trustworthy for this application [3].
Solution:
- Switch to a GLS or Bayesian framework. Implement a regression that accounts for the full covariance structure [3].
- Use validated software. Employ specialized open-source tools like the "kinisi" Python package, which is designed for this precise problem and uses a robust Bayesian approach to provide accurate uncertainty estimates [3].
- Model the covariance. If building your own analysis, use a model covariance matrix Σ′ for a freely diffusing system, parametrized with your data, within the GLS framework [3].
Issue 2: Poor Quality Fit to MSD Data
Problem: The linear fit, regardless of method, does not align well with the calculated MSD points, or the fit residual shows a clear systematic pattern.
Diagnosis: The underlying assumption of pure, simple Brownian motion may be incorrect. The system might exhibit more complex dynamics, such as anomalous diffusion, confinement, or directional flow.
Solution:
- Visual inspection. Plot your raw MSD data and the fitted line. Check the residual plot (difference between MSD data and the fit) for any non-random patterns.
- Test for alternative models. Fit your data to models for anomalous diffusion (MSD ~ t^α) or confined diffusion. A systematic comparison of model classes can be conducted using methods like Bayesian model selection, which helps identify the most plausible model given the data [82].
- Segment your trajectory. If you suspect the particle undergoes different diffusion regimes during a single trajectory, use methods to detect these changes before attempting to fit a single diffusion coefficient to the entire dataset [29].
Research Reagent Solutions
Table 1: Essential Computational Tools for MSD and GLS Analysis
| Tool / Resource | Primary Function | Key Application in Analysis |
|---|---|---|
| GLS Regression Algorithm | Estimates unknown parameters in a linear regression model when residuals are correlated and/or heteroscedastic [81]. | The core mathematical procedure for obtaining an optimal, statistically efficient estimate of the diffusion coefficient from correlated MSD data [3]. |
| Covariance Matrix (Σ) | Describes the variances and covariances between all pairs of MSD values in the time series [3]. | In GLS, its inverse (Ωâ»Â¹) is used to weight the regression, correctly accounting for the correlation structure and heteroscedasticity of the MSD data [3] [81]. |
| Bayesian Regression | Provides a posterior probability distribution for model parameters (like the diffusion coefficient) rather than a single point estimate [3]. | An alternative to GLS that naturally incorporates uncertainty; its mean posterior estimate is equal to the GLS solution when using an uninformative prior [3]. |
| Model Class Selection | A framework to compare different candidate models (e.g., uncorrelated, spatially correlated, temporally correlated error) and select the most plausible one [82]. | Helps identify the correct correlation structure for the measurement error, which is critical for constructing an accurate covariance matrix [82]. |
Experimental Protocols
Protocol 1: Estimating the Self-Diffusion Coefficient using GLS
This protocol outlines the steps for a Generalized Least Squares analysis of Mean Squared Displacement data.
1. Calculate the Observed MSD:
- For a simulation or trajectory of equivalent particles, compute the MSD vector x using the standard formula, which is an average over equivalent particles and time origins [3]:
x(t) = (1/N(t)) * Σ [r_i(t + Δt) - r_i(t)]²- where
N(t)is the total number of observed squared displacements at time lagt.
2. Approximate the Covariance Matrix (Σ):
- The true covariance matrix is unknown. Use a model covariance matrix Σ′ derived for an equivalent system of freely diffusing particles [3].
- Parametrize this model covariance matrix using the statistics from your observed simulation data [3].
3. Perform GLS Regression:
- Construct the model matrix A = [1, t], where t is the vector of observed time lags [3].
- Calculate the GLS estimate for the linear model parameters (slope and intercept) using the formula [3]:
β̂ = (Aáµ€ Σ′â»Â¹ A)â»Â¹ Aáµ€ Σ′â»Â¹ x
- The slope of the linear fit is related to the self-diffusion coefficient D* via the Einstein relation:
slope = 6D*(in 3 dimensions) [3].
4. Estimate Uncertainty:
- The covariance of the estimated parameters is given by
Cov[β̂] = (Aáµ€ Σ′â»Â¹ A)â»Â¹[3] [81]. - Use this to determine the standard error or confidence intervals for the fitted diffusion coefficient.
Protocol 2: Optimal Point Selection for MSD Fitting
This protocol is particularly useful for single-particle tracking data with non-negligible localization error [29].
1. Calculate the Reduced Localization Error (x):
- Estimate your localization uncertainty, σ, from the photon count and Point Spread Function (PSF) dimensions [29].
- Calculate the reduced localization error: x = σ² / (D_est Δt), where
D_estis a preliminary estimate of the diffusion coefficient (e.g., from a two-point MSD fit) andΔtis the frame duration [29].
2. Determine the Optimal Number of Points (p_min):
- The optimal number of MSD points, p_min, to use in the fit is a function of x and the total number of points in the trajectory, N [29].
- Consult the theoretical or empirical expressions described in the literature (e.g., [29]) to find p_min for your specific x and N.
3. Perform the Fit:
- Fit a linear model to the first p_min points of your MSD curve.
- Note: This method is presented as a robust alternative when the full covariance matrix for GLS is difficult to estimate, and it can perform equivalently to a weighted fit when p_min is chosen correctly [29].
Workflow Visualization
The following diagram illustrates the logical workflow and decision points for selecting an optimal fitting strategy for MSD data.
Diagram 1: Workflow for optimal MSD fitting.
Handling Heteroscedasticity and Serial Correlation in Time-Series Data
Frequently Asked Questions (FAQs)
1. What are heteroscedasticity and serial correlation, and why are they problematic in time-series analysis?
Heteroscedasticity occurs when the variance of the regression errors is not constant across observations [83] [84]. Serial Correlation (or Autocorrelation) occurs when regression errors are correlated across time periods [83] [84]. Both violate standard ordinary least squares (OLS) assumptions. Heteroscedasticity does not bias coefficient estimates but makes standard errors unreliable, inflating t-statistics and compromising statistical inference [83]. Serial correlation can cause OLS standard errors to underestimate the true standard errors, leading to overly narrow confidence intervals and an increased risk of Type I errors (false positives) [83].
2. How can I quickly check if my time-series data suffers from these issues?
Visual inspection of residual plots is a good starting point. For heteroscedasticity, plot residuals against fitted values; a fan-shaped pattern suggests heteroscedasticity [85]. For serial correlation, plot residuals over time; patterns or trends indicate correlation [83]. Formal tests are essential for confirmation.
3. My primary goal is prediction, not inference. Do I still need to correct for these problems?
While flawed standard errors may not directly affect the predicted values themselves, addressing these issues can lead to more accurate prediction intervals. Furthermore, if autocorrelation is present, model specifications that account for it (e.g., including lagged variables) can improve forecast accuracy by capturing dynamic patterns in the data [85].
4. Should I address heteroscedasticity or serial correlation first?
There is no strict rule, and the problems often coexist. Some modern approaches, like using HAC (Heteroskedasticity and Autocorrelation Consistent) standard errors, correct for both simultaneously [83] [86]. A joint test for both conditions can also be performed [86]. If using a stepwise approach, modeling the autocorrelation structure often takes precedence in time-series data, as it directly relates to the data-generating process.
5. Can these issues affect research on diffusion coefficients?
Absolutely. Accurate parameter estimation and uncertainty quantification are crucial in modeling diffusion processes. If experimental data is collected over time, serial correlation in measurement errors can lead to incorrect conclusions about the significance of factors affecting diffusion. Heteroscedasticity, where measurement variance changes with concentration or time, similarly invalidates standard error estimates [87] [88] [89].
Troubleshooting Guides
Guide 1: Diagnosing Heteroscedasticity and Serial Correlation
Follow this workflow to diagnose common issues in your time-series regression model.
Step 1: Run Initial Model & Obtain Residuals After fitting your initial regression model, save the residuals (errors) for analysis.
Step 2: Visual Inspection Create the following plots:
- Residuals vs. Fitted Values: Check for a random scatter. A funnel-shaped pattern (variance increases/decreases with fitted values) suggests heteroscedasticity [85].
- Residuals vs. Time (or Order): Check for randomness. A pattern, such as a run of positive residuals followed by a run of negative residuals, suggests positive serial correlation [83].
- ACF (Autocorrelation Function) Plot of Residuals: Significant bars at lag 1 or higher indicate serial correlation.
Step 3: Formal Statistical Testing
- For Heteroscedasticity: Use the Breusch-Pagan Test [83] [85] [84].
- Null Hypothesis (Hâ‚€): Homoskedasticity (constant error variance).
- Test Statistic: ( BP = n \times R^{2} \sim \chi^{2}_{k} ) where
nis the sample size and ( R^{2} ) comes from an auxiliary regression of squared residuals on the independent variables [83]. - Interpretation: A significant p-value (e.g., <0.05) leads to a rejection of Hâ‚€, indicating heteroscedasticity.
- For Serial Correlation: Use the Durbin-Watson Test [83] [85] [84].
- Null Hypothesis (Hâ‚€): No first-order serial correlation.
- Test Statistic: ( DW \approx 2(1 - \hat{\rho}) ), where (\hat{\rho}) is the estimated correlation between consecutive residuals [83].
- Interpretation:
- ( DW \approx 2 ): Suggests no autocorrelation.
- ( DW < 2 ): Suggests positive autocorrelation (common in time series).
- ( DW > 2 ): Suggests negative autocorrelation.
- Compare the calculated DW statistic to critical values from Durbin-Watson tables ((dl) and (du)) for a formal decision [83].
Guide 2: Correcting for Heteroscedasticity
If diagnostics confirm heteroscedasticity, here are the primary remediation methods.
1. Robust Standard Errors (White-Huber Standard Errors): This is the most common and straightforward solution. It recalculates the standard errors of the coefficients to be consistent in the presence of heteroscedasticity, without changing the coefficient estimates themselves [83]. This method is ideal when you want to maintain your original model but obtain valid inference (t-tests, confidence intervals).
- Implementation: Most statistical software (R, Python, Stata) have built-in functions to compute robust standard errors after OLS regression.
2. Generalized Least Squares (GLS): This method transforms the original regression equation to eliminate heteroscedasticity. It requires specifying a model for the variance structure (e.g., variance proportional to one of the independent variables). GLS provides efficient (minimum variance) estimators if the variance structure is correctly specified [83].
3. Variable Transformation: Transforming the dependent variable (e.g., using the natural logarithm,
ln(y)) can sometimes stabilize the variance. This approach can also help normalize the error distribution but changes the interpretation of the coefficients.
Guide 3: Correcting for Serial Correlation
If diagnostics confirm serial correlation, consider these corrective measures.
1. Cochrane-Orcutt or Hildreth-Lu Procedures: These are iterative methods that estimate the autocorrelation parameter ((\rho)) and transform the data to remove the correlation before re-estimating the model [85].
2. Include Lagged Variables: A powerful and intuitive approach is to model the dependency directly.
- Autoregressive (AR) Terms: Include lagged values of the dependent variable as predictors (e.g., ( y_{t-1} )).
- Lagged Independent Variables: Include lagged values of the independent variables. This approach often has a clear theoretical justification in time-series contexts.
3. Newey-West (HAC) Standard Errors: Similar to robust standard errors for heteroscedasticity, Newey-West standard errors are "heteroskedasticity and autocorrelation consistent" (HAC). They correct the standard errors for both heteroscedasticity and a certain amount of serial correlation, without changing the OLS coefficients [83] [86]. This is a popular "model-free" correction for inference.
Quantitative Data & Error Metrics
The table below summarizes key error metrics used to evaluate model performance, such as when comparing models before and after correcting for heteroscedasticity or serial correlation, or when assessing forecasting accuracy [90] [91].
Table 1: Common Error Metrics for Model Evaluation & Forecast Accuracy
| Metric | Formula | Interpretation | Best For | ||
|---|---|---|---|---|---|
| Mean Absolute Error (MAE) | ( MAE = \frac{1}{n}\sum_{i=1}^{n} | yi - \hat{y}i | ) | Average absolute error. Easy to understand. | Assessing accuracy on a single series where penalizing outliers is not a priority [90] [91]. |
| Root Mean Squared Error (RMSE) | ( RMSE = \sqrt{\frac{1}{n}\sum{i=1}^{n}(yi - \hat{y}_i)^2} ) | Square root of the average squared error. Sensitive to outliers. | Model optimization and comparison when error distribution is Gaussian; penalizes large errors [90] [91]. | ||
| Mean Absolute Percentage Error (MAPE) | ( MAPE = \frac{100\%}{n}\sum_{i=1}^{n} | \frac{yi - \hat{y}i}{y_i} | ) | Average absolute percentage error. Scale-independent. | Comparing forecast performance across different time series, but problematic if y is close to zero [90] [91]. |
Experimental Protocol: Linking to Diffusion Coefficient Research
The following protocol is adapted from research on measuring drug diffusion coefficients, a context where precise error estimation is critical [87].
Aim: To determine the diffusion coefficient (D) of a pharmaceutical compound (e.g., Theophylline) through an artificial mucus layer using time-resolved Fourier Transform Infrared (FTIR) spectroscopy.
Background: Inhaled drugs must diffuse through the pulmonary mucus to reach their site of action. The diffusion coefficient quantifies the rate of this transport and is vital for pharmacokinetic modeling and drug design [87].
Materials:
- Research Reagent Solutions:
- Artificial Mucus: A synthetic hydrogel that mimics the physicochemical properties of human pulmonary mucus [87].
- Drug Solution: A known concentration of the drug of interest (e.g., Theophylline or Albuterol) in an appropriate solvent [87].
- ATR Crystal: A Zinc Selenide (ZnSe) crystal serving as the internal reflection element for the FTIR spectrometer [87].
Methodology:
- Experimental Setup: Place the artificial mucus layer in direct contact with the ATR crystal. The upper surface of the mucus is then brought into contact with the drug solution.
- Data Collection: Collect FTIR spectra at constant time intervals. Monitor the change in intensity of a functional group-specific peak for the drug.
- Calibration: Establish a relationship between peak height (or area) and drug concentration using Beer-Lambert Law [87].
- Modeling and Estimation: The concentration profile over time is analyzed using Fick's 2nd Law of Diffusion. A solution to this law (e.g., Crank's trigonometric series for a planar semi-infinite sheet) is fitted to the experimental data to determine the diffusion coefficient,
D[87].
Statistical & Error Considerations:
- The time-series data of concentration will likely exhibit serial correlation, as the concentration at time
tis highly dependent on the concentration at timet-1. - Heteroscedasticity may also be present if measurement variance changes with concentration levels.
- Recommended Approach: Use a GLS estimator that explicitly models the error structure (e.g., an AR(1) process for the errors) when fitting the diffusion model. This provides efficient estimates of
Dand valid confidence intervals for the parameter [83] [86]. The error metrics from Table 1 can be used to assess the goodness-of-fit of the diffusion model.
The Scientist's Toolkit
Table 2: Essential Reagents & Materials for Diffusion Experiments
| Item | Function in Experiment |
|---|---|
| Artificial Mucus | A synthetic hydrogel that replicates the viscous, hydrophobic, and cross-linked network of native mucus, providing a standardized medium for diffusion studies [87]. |
| ATR-FTIR Spectrometer | Enables non-invasive, time-resolved chemical analysis of the diffusion process by measuring infrared spectra of molecules in contact with the ATR crystal [87]. |
| Model Drug Compounds (e.g., Theophylline, Albuterol) | Well-characterized pharmaceutical compounds used as probes to study and quantify transport phenomena through biological barriers [87]. |
| Zinc Selenide (ZnSe) ATR Crystal | An optically dense crystal that allows for total internal reflection of the IR beam, creating an evanescent wave that penetrates the sample in contact with it [87]. |
Benchmarking and Validation: Ensuring Data Reliability
Validating Computational Predictions with Experimental Data
Frequently Asked Questions (FAQs)
Q1: What is the primary reason my computational predictions fail to match my experimental results? A common reason is that the training data and the experimental data are not independent and identically distributed (i.i.d.). In spatial or temporal contexts like diffusion research, traditional validation methods often fail because they assume data independence. If your validation data comes from a different distribution than your test conditions (e.g., different compositional ranges or temperatures), the validation will be inaccurate [92]. Always ensure your computational training set is representative of your experimental conditions.
Q2: How can I validate a computational model when experimental data is limited or expensive to obtain? When experimental data is scarce, employ a combination of computational validation techniques to build confidence before costly experiments. This includes:
- Retrospective Clinical Analysis: Using existing databases (e.g., clinicaltrials.gov) or electronic health records to find supporting evidence for predictions [93].
- Literature Mining: Systematically searching published literature for prior experimental support of the predicted connection [93].
- Benchmarking: Testing your model's performance on standardized, high-quality datasets relevant to your field [93].
Q3: What are the best practices for ensuring my data is valid before starting computational analysis? Follow a structured data validation process to maintain data integrity [94]:
- Define Clear Rules: Establish specific, predefined criteria for data format, range, and consistency.
- Use Automated Tools: Implement software for data cleansing, standardization, and validation.
- Validate at Multiple Stages: Check data quality during extraction, transformation, and loading (ETL) processes.
- Monitor and Update: Continuously review and update validation rules as data and research needs evolve.
Q4: What is the difference between analytical validation and clinical validation in a context like drug development?
- Analytical Validation focuses on the technical performance of the computational method itself, using metrics like sensitivity and specificity to show it is functioning as intended [93].
- Clinical Validation demonstrates that the model provides a genuine clinical benefit, typically requiring prospective evaluation or randomized controlled trials to prove it improves patient outcomes in a real-world setting [95]. A model can be analytically valid but not clinically useful.
Q5: Why is error analysis crucial, and how do I move beyond a single aggregate accuracy score? Aggregate accuracy can hide significant model weaknesses. Error Analysis is essential to identify specific conditions where your model fails. You should [96]:
- Identify Error Cohorts: Use techniques like decision trees or heatmaps to discover data subgroups with disproportionately high error rates.
- Diagnose Root Causes: Explore data distributions and use model interpretability tools to understand why errors occur in these cohorts, such as under-represented data or noisy labels.
Troubleshooting Guides
Issue 1: Discrepancy Between Predicted and Experimentally Measured Diffusion Coefficients
Problem: Your computational model predicts diffusion coefficients that are inconsistent with values measured experimentally, for example, in a multi-principal element alloy like NiCoFeCrAl.
Potential Causes and Solutions:
| Cause | Diagnostic Steps | Solution |
|---|---|---|
| Inappropriate Model Assumptions | Review the theoretical foundations of your model. Check if it accounts for effects like the vacancy wind effect, which can be significant for intrinsic diffusion coefficients [97]. | Use a more sophisticated model that incorporates key atomic-level interactions and cross-diffusion effects. Validate first on a simpler system with known parameters. |
| Non-Intersecting Diffusion Paths | Analyze the design of your diffusion couples. In multicomponent systems, standard methods may not allow for the exact intersection of diffusion paths in composition space, making estimation impossible [97]. | Employ an inventive design strategy, such as using pseudo-binary or pseudo-ternary diffusion couples, to constrain and intersect diffusion paths for reliable coefficient estimation [97]. |
| Incorrect Dependent Variable Selection | Calculate the main interdiffusion coefficients using different elements as the dependent variable. A different or opposite trend in relative diffusivities indicates this issue [97]. | Report tracer diffusion coefficients (e.g., DNi*, DAl*) to describe the actual atomic mechanism of diffusion, as they are not dependent on the reference element choice [97]. |
Experimental Protocol: Estimating Tracer Diffusion Coefficients via Designed Diffusion Couples This methodology allows for the purely experimental estimation of tracer, intrinsic, and interdiffusion coefficients in complex multicomponent systems [97].
- Design: Fabricate specialized diffusion couples (e.g., pseudo-binary or pseudo-ternary) that are designed to intersect diffusion paths within the Gibbs polyhedron of the multicomponent system.
- Annealing: Heat-treat the diffusion couples at the target temperature for a predetermined time in an inert atmosphere to allow for sufficient interdiffusion.
- Characterization: Use electron probe microanalysis (EPMA) to obtain precise composition profiles across the interdiffusion zone of the couple.
- Calculation: Apply the relevant equations (e.g., the Boltzmann-Matano method or its derivatives) to the composition profiles to extract the interdiffusion fluxes and coefficients at the intersection point.
- Derivation: Leverage thermodynamic data and the estimated interdiffusion coefficients to calculate the more fundamental tracer diffusion coefficients.
Issue 2: Unacceptably High Error Rates in a Specific Data Cohort
Problem: Your overall model accuracy is good, but it performs poorly for a specific subgroup of data (e.g., a specific alloy composition or a patient demographic).
Diagnosis and Resolution Workflow:
Issue 3: Computational Drug Repurposing Prediction Lacks Experimental Support
Problem: You have a list of computational drug repurposing candidates, but you need to prioritize which ones to validate experimentally.
Validation Strategy Table: The following table outlines types of validation, ordered from least to most rigorous, that can provide supporting evidence for computational predictions [93].
| Validation Type | Description | Strength | Weakness |
|---|---|---|---|
| Literature Support | Manual or automated search of biomedical literature for existing connections between the drug and disease. | Quick, easy, leverages public knowledge. | Prone to bias; does not provide new evidence. |
| Public Database Search | Querying databases for known drug-target-disease interactions (e.g., clinicaltrials.gov). | Provides context on existing clinical development. | Does not validate novel predictions. |
| Retrospective Clinical Analysis | Using real-world data like Electronic Health Records (EHR) to find evidence of off-label efficacy. | Strong evidence of effect in humans. | Privacy and data accessibility issues; confounding factors. |
| In Vitro/Ex Vivo Experiments | Testing the drug candidate on cell lines or tissue samples in a controlled lab environment. | Provides direct biological evidence; controls environment. | May not translate to more complex in vivo systems. |
| In Vivo Experiments | Testing the drug candidate in animal models of the disease. | Tests efficacy in a whole, living organism. | Ethical considerations; cost and time intensive. |
| Prospective Clinical Trials | Designing and executing a new clinical trial to test the drug candidate for the new indication. | The gold standard for validation. | Extremely costly, time-consuming, and high-risk. |
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for Diffusion Coefficient Experiments
| Item | Function |
|---|---|
| Multi-principal Element Alloy Ingots | The base materials for creating diffusion couples, with high-purity elements to form solid solution alloys like NiCoFeCrAl [97]. |
| Diffusion Couple Assembly Jig | A specialized fixture used to align and apply pressure to the two metal blocks being bonded, ensuring a perfectly flat, intimate interface before annealing. |
| High-Temperature Vacuum Furnace | An annealing furnace capable of maintaining precise temperatures (often >1000°C) in an inert or vacuum atmosphere to prevent oxidation during diffusion. |
| Electron Probe Microanalyzer (EPMA) | An instrument that uses a focused electron beam to generate X-rays from a sample, providing highly precise quantitative composition measurements across the diffusion zone [97]. |
| Metallographic Polishing Setup | Equipment and consumables (e.g., SiC paper, diamond paste) for preparing smooth, scratch-free cross-sectional surfaces of the diffusion couple for accurate EPMA analysis. |
Frequently Asked Questions
1. Under what conditions is Ordinary Least Squares (OLS) the appropriate method to use? OLS is the appropriate default method when your data satisfies its key classical assumptions: the relationship between variables is linear in the coefficients, the error term has a constant variance (homoscedasticity), and observations of the error term are uncorrelated with each other (no autocorrelation) [78]. When these assumptions hold true, OLS produces the best possible unbiased and efficient estimates [78].
2. My data shows non-constant variance. Which method should I use? If your data exhibits heteroscedasticity—where the variance of the errors is not constant—Weighted Least Squares (WLS) is the recommended approach [98] [99]. WLS accounts for this by giving less weight to observations with higher variance and more weight to those with lower variance, thus providing a more reliable estimate than OLS under these conditions [98].
3. How do I handle data where errors are correlated, such as in time-series measurements? For data with correlated errors, such as time-series or spatially correlated data, Generalized Least Squares (GLS) is designed to handle this issue [98] [3]. GLS explicitly models the correlation structure among the error terms, which leads to statistically efficient estimates and accurate uncertainty quantification, unlike OLS or WLS [3].
4. What is the main advantage of using Bayesian Regression over traditional methods like OLS? The primary advantage of Bayesian Regression is its ability to seamlessly incorporate prior knowledge or existing data into the analysis, resulting in a posterior distribution that directly quantifies the probability of parameter values [37] [100]. This is particularly valuable when you have informative prior information, or when you want to make direct probability statements about your parameters, such as "there is a 95% probability that the diffusion coefficient lies within a certain interval" [3] [100].
5. Are there computational drawbacks to using Bayesian Regression? Yes, Bayesian methods are often more computationally intensive and complex to implement than traditional least-squares approaches [100]. They typically require Markov Chain Monte Carlo (MCMC) sampling to approximate the posterior distribution, which can be slow for very large datasets, and they demand additional knowledge of Bayesian programming and specific software [3] [100].
Troubleshooting Guides
Problem: The uncertainty in my estimated diffusion coefficient seems unrealistically small.
- Possible Cause: This is a common issue when using OLS regression on Mean Squared Displacement (MSD) data from simulations. The OLS method assumes independent and identically distributed errors, but MSD data is inherently both heteroscedastic and serially correlated [3]. Using OLS under these conditions leads to a significant underestimation of the true uncertainty [3].
- Solution: Shift to a method that accounts for the true correlation structure.
- Recommended Method: Use Generalized Least Squares (GLS) or Bayesian Regression with a modeled covariance matrix [3].
- Protocol:
- Calculate the observed MSD vector from your trajectory data [3].
- Approximate the covariance matrix (Σ) of the MSD, for instance, using an analytical model for freely diffusing particles [3].
- For GLS: Fit the linear model using the GLS estimator,
β̂ = (AᵀΣâ»Â¹A)â»Â¹AᵀΣâ»Â¹x, whereAis your model matrix [3]. - For Bayesian Regression: Use MCMC sampling to obtain the posterior distribution of the slope (which is proportional to the diffusion coefficient), using the likelihood function for a multivariate normal distribution [3].
Problem: My regression results are being overly influenced by a few unreliable data points.
- Possible Cause: Some measurements in your dataset are noisier or less reliable than others, and the OLS model is treating all observations as equally trustworthy [98].
- Solution: Apply Weighted Least Squares (WLS) to down-weight the influence of less reliable data.
- Recommended Method: WLS regression.
- Protocol:
- Identify a suitable weighting scheme based on the known reliability of your data. A common choice is to set the weights as the reciprocal of the variance at each point (e.g.,
weights = 1 / (data['Hours']2)as in [98]). - Fit the regression model using the WLS function from your statistical software, providing the vector of weights [98].
- The resulting fit will be more robust to the noisy data points, as the model now "trusts" the more reliable data more [98].
- Identify a suitable weighting scheme based on the known reliability of your data. A common choice is to set the weights as the reciprocal of the variance at each point (e.g.,
Problem: I have valuable prior knowledge from previous experiments that I want to include in my current analysis.
- Possible Cause: You are using a frequentist method (OLS, WLS, GLS) that only uses the data from the current experiment and does not provide a framework for incorporating external information [37] [101].
- Solution: Use Bayesian Regression to formally integrate your prior knowledge.
- Recommended Method: Bayesian Linear Regression.
- Protocol:
- Formalize your prior knowledge about the parameters (e.g., the diffusion coefficient and intercept) into prior probability distributions. For example, if you know a diffusion coefficient should be positive, you can use a prior that excludes negative values [100].
- Define the likelihood function for your observed data, typically as a normal distribution centered on your linear model.
- Use software (e.g., PyMC3, Stan) to compute the posterior distribution via Bayes' Theorem [3].
- The result is a full posterior distribution for your parameters, which combines your prior knowledge with the new evidence from your data [101].
Comparison of Estimation Methods
The following table summarizes the key characteristics, assumptions, and typical use cases for each regression method in the context of estimating parameters like diffusion coefficients.
| Feature | Ordinary Least Squares (OLS) | Weighted Least Squares (WLS) | Generalized Least Squares (GLS) | Bayesian Regression |
|---|---|---|---|---|
| Core Principle | Minimizes the sum of squared residuals, giving equal weight to all data points [98]. | Minimizes the weighted sum of squared residuals to account for unequal variance [98]. | Minimizes a generalized squared residual form that accounts for both non-constant variance and error correlation [3]. | Uses Bayes' Theorem to combine prior knowledge with observed data to form a posterior distribution [3]. |
| Key Assumptions | Linear model, homoscedasticity, uncorrelated errors [78]. | Linear model, uncorrelated errors, but can handle heteroscedasticity [99]. | Linear model; can handle both heteroscedasticity and correlated errors when the covariance matrix is known or estimated [3] [99]. | Linear model, specification of a likelihood and prior distributions [101]. |
| Handling of Prior Info | No mechanism for incorporating prior information. | No mechanism for incorporating prior information. | No mechanism for incorporating prior information. | Explicitly incorporates prior knowledge through prior distributions [37] [100]. |
| Output | Single point estimates for coefficients and their standard errors. | Single point estimates for coefficients and their standard errors. | Single point estimates for coefficients and their standard errors. | Full posterior probability distribution for the coefficients [3]. |
| Uncertainty Quantification | Can underestimate true uncertainty if assumptions are violated [3]. | Can still underestimate uncertainty if correlations are present [3]. | Provides accurate uncertainty estimates when the covariance structure is correct [3]. | Provides natural and direct uncertainty quantification via the posterior distribution [3] [100]. |
| Ideal Use Case | The default method for clean, homoscedastic, and independent data [78] [99]. | Data with known or suspected heteroscedasticity where different observations have different reliability [98]. | Data with correlated errors (e.g., time-series, spatial data) or complex covariance structures [98] [3]. | Incorporating previous experimental results, handling complex models, or when a full probabilistic assessment is desired [37] [3]. |
Experimental Protocols for Diffusion Coefficient Estimation
Protocol 1: Standard OLS and GLS Workflow for MSD Analysis
This protocol outlines the steps for estimating the self-diffusion coefficient (D*) from molecular dynamics trajectories using both OLS and the more robust GLS method [3].
Step-by-Step Instructions:
- Calculate Observed MSD: From your particle trajectory, compute the Mean Squared Displacement (MSD) as a function of time. The MSD at time
tis calculated by averaging the squared displacements of all equivalent particles over all available time origins within the trajectory [3]. - Fit a Linear Model: According to the Einstein relation, the MSD is linear in time:
⟨Δr(t)²⟩ = 6D*t + c. The slope of this line is proportional to the self-diffusion coefficient,D*[3].- For OLS: Use a standard linear regression (e.g.,
sm.OLS(y, X).fit()in Python's statsmodels) to fit the lineMSD ~ t[98]. The slope of this fit is your estimateD̂*_OLS. - For GLS: You must first approximate the covariance matrix (Σ) of the MSD values. This matrix captures the heteroscedastic and correlated nature of the MSD data. You can use an analytical model for a freely diffusing system, parametrized with your data. Then, perform the GLS regression using this covariance matrix (e.g.,
sm.GLS(y, X, sigma=Sigma).fit()) [3].
- For OLS: Use a standard linear regression (e.g.,
- Extract D* and Uncertainty:
- From the OLS fit, the estimated slope is
6 * DÌ‚*_OLS. The standard error of the slope is provided by the model, but it is likely an underestimate [3]. - From the GLS fit, the estimated slope is
6 * DÌ‚*_GLS. The standard error from the GLS model is a more accurate representation of the true statistical uncertainty in your estimate [3].
- From the OLS fit, the estimated slope is
Protocol 2: Bayesian Regression for MSD Analysis with Informed Priors
This protocol is advantageous when you have prior knowledge, such as a plausible range for the diffusion coefficient from earlier experiments or simulations [3].
Step-by-Step Instructions:
- Specify Prior Distributions: Quantify your prior knowledge about the parameters (the slope
mrelated toD*and the interceptc) as probability distributions. For example:- If you know
D*should be positive and around1.0 × 10â»âµ cm²/s, you could use a Gamma distribution or a Normal distribution with a positive constraint centered near that value. - If you have little prior information, you can use "weakly informative" or "flat" priors that impose only basic constraints (e.g., positivity) [100].
- If you know
- Define the Likelihood Function: This represents the probability of observing your MSD data given a specific linear model. It is typically modeled as a multivariate normal distribution:
X ~ MVNormal(A * β, Σ), whereXis the MSD vector,Ais the design matrix,βcontains the slope and intercept, andΣis the covariance matrix [3]. - Compute the Posterior Distribution: Use Markov Chain Monte Carlo (MCMC) sampling methods (e.g., using PyMC3, Stan, or the
kinisipackage) to draw samples from the joint posterior distribution of the parameters,p(m, c | X). This distribution is proportional to the prior times the likelihood [3]. - Analyze the Posterior: The MCMC samples provide a full empirical distribution for your parameters.
- The mean or median of the sampled slopes can be used as your point estimate for
D*. - The 2.5th and 97.5th percentiles of these samples form a 95% credible interval, which you can directly interpret as: "There is a 95% probability that the true diffusion coefficient lies within this interval," given your prior and your data [3] [100].
- The mean or median of the sampled slopes can be used as your point estimate for
Research Reagent Solutions
The following table lists key computational tools and conceptual components essential for implementing the regression methods discussed, particularly in the context of diffusion research.
| Item Name | Function / Application |
|---|---|
| Covariance Matrix (Σ) | A core component for GLS and Bayesian regression. It quantifies the variances and covariances of the MSD data points, capturing the heteroscedastic and correlated error structure. It is essential for achieving statistically efficient estimates [3]. |
| Prior Distribution | A key "reagent" in Bayesian analysis. It is a probability distribution that formalizes pre-existing knowledge or assumptions about the model parameters (like the diffusion coefficient) before the current data is observed [37] [100]. |
| Markov Chain Monte Carlo (MCMC) | A computational algorithm used in Bayesian statistics to draw samples from the complex posterior distribution when an analytical solution is infeasible. It is the workhorse for practical Bayesian inference [3]. |
| Statsmodels Library (Python) | A comprehensive Python module for estimating and analyzing statistical models, including OLS, WLS, GLS, and (in some cases) basic Bayesian models. It is ideal for implementing the classical regression methods [98]. |
| Kinisi Package | An open-source Python package specifically designed for the analysis of kinetics and diffusion data from simulations. It implements the Bayesian regression method described in [3] for robust estimation of diffusion coefficients [3]. |
| Mean Squared Displacement (MSD) | The primary input data for estimating the diffusion coefficient. It is calculated from particle trajectories and fitted to a linear model via the Einstein relation [3]. |
Frequently Asked Questions
1. What are the most common pitfalls when using MSD analysis for anomalous diffusion? The most common pitfalls include using trajectories that are too short, which introduces significant statistical error, and applying Ordinary Least-Squares (OLS) regression to MSD data, which neglects the data's inherent serial correlation and heteroscedasticity (unequal variance). OLS leads to statistically inefficient estimates and, crucially, significantly underestimates the uncertainty in the calculated diffusion coefficient, creating false confidence in the results [3].
2. My trajectories are short due to experimental constraints. How can I accurately determine the diffusion coefficient? For short trajectories, traditional MSD analysis becomes highly unreliable [102]. The recommended approach is to use methods that account for the full statistical properties of the data. Bayesian regression and Generalized Least-Squares (GLS) are statistically efficient as they incorporate the covariance structure of the MSD, providing more reliable estimates and accurate uncertainty quantification from a single, finite trajectory [3]. Furthermore, machine-learning-based methods have shown superior performance in analyzing short or noisy trajectories [102].
3. How does trajectory length impact the accuracy of my diffusion coefficient measurement? Trajectory length has a direct and profound impact on accuracy. Experimental research has demonstrated that to achieve an accuracy of approximately 10% for the diffusion coefficient, trajectories comprising about 1000 data points are required. Using shorter segments, such as 100-point trajectories, can lead to relative errors of 25% or more [103]. There is an optimal number of MSD points to use for fitting, which depends on the total trajectory length [103].
4. Beyond trajectory segmentation, what other methods can detect heterogeneous or changing diffusion? The field has moved beyond simple MSD fitting. The 2nd Anomalous Diffusion (AnDi) Challenge benchmarked many modern methods designed to identify changepoints (CPs) where diffusion properties, like the coefficient (D) or exponent (α), change within a single trajectory [104]. These include ensemble methods that characterize an entire set of trajectories and single-trajectory methods that can pinpoint the exact location of a change in dynamic behavior [104].
5. Are there experimental techniques beyond single-particle tracking to measure drug diffusion coefficients? Yes, several powerful techniques exist. UV Imaging utilizes a drug's UV absorbance to map its concentration distribution in real-time. By fitting the solution of Fick's second law to the concentration profile, one can simultaneously determine both the solubility and diffusion coefficient of a drug in a matter of minutes [105]. Attenuated Total Reflectance Fourier Transform Infrared Spectroscopy (ATR-FTIR) is another non-invasive method that monitors diffusion by tracking changes in infrared spectra correlated to drug concentration via Beer's Law [87].
Troubleshooting Guides
Problem: Inaccurate or Inconsistent Diffusion Coefficients from MSD Analysis
Potential Causes and Solutions:
Cause: Short Trajectories.
- Solution: Use specialized analysis methods. For very short trajectories (tens of points), leverage machine-learning classifiers that have been trained on a wide variety of diffusion models [102]. For short but analyzable trajectories, employ Bayesian regression or GLS instead of OLS to maximize the information extracted from limited data [3].
Cause: Improper Statistical Fitting (using OLS).
- Solution: Replace OLS with a more robust fitting procedure. The recommended workflow is:
- Calculate the MSD from your trajectory.
- Use a fitting method that accounts for the covariance (Σ) of the MSD data, such as Generalized Least-Squares (GLS) or Bayesian regression [3].
- Tools like the
kinisiPython package are designed specifically for this purpose and can provide an optimal estimate of D* and its uncertainty [3].
- Solution: Replace OLS with a more robust fitting procedure. The recommended workflow is:
Cause: Heterogeneous Diffusion (Changepoints).
- Solution: Apply changepoint detection algorithms. Use methods benchmarked in the AnDi Challenge that are designed to segment a single trajectory into portions with distinct diffusion coefficients or anomalous exponents [104]. Do not analyze a heterogeneous trajectory as a single unit.
Problem: Low Resolution in Detecting Anomalous Diffusion Exponents
Potential Causes and Solutions:
Cause: Confounding Effects from Motion Heterogeneity.
- Solution: Carefully interpret the anomalous exponent α. Apparent anomalous diffusion can be caused by a particle switching between different normal diffusion states (e.g., due to transient binding). Use analysis methods that can distinguish between genuine anomalous diffusion and heterogeneity-induced apparent anomaly [104].
Cause: Low Signal-to-Noise Ratio or Localization Error.
- Solution: Incorporate localization precision estimates into your model. The presence of noise systematically biases the estimation of the anomalous exponent α [102]. Use models that explicitly include and correct for the known localization error to obtain an unbiased estimate of the true diffusion parameters [102].
Table 1: Impact of Trajectory Length on Diffusion Coefficient Accuracy (from Single-Particle Tracking)
| Trajectory Length (Data Points) | Relative Error in D | Recommendation |
|---|---|---|
| ~100 points | ~25% or higher | Use with extreme caution; requires advanced ML or statistical methods. |
| ~1000 points | ~10% | A common target for achieving reliable accuracy [103]. |
| >1.5 x 105 points | Used for benchmarking | Enables decomposition into many shorter segments for statistical analysis [103]. |
Table 2: Comparison of MSD Fitting Methods for Diffusion Coefficient Estimation
| Fitting Method | Statistical Efficiency | Handles Correlated Data? | Uncertainty Estimation | Recommendation |
|---|---|---|---|---|
| Ordinary Least-Squares (OLS) | Low | No | Severely underestimated [3] | Not recommended. |
| Weighted Least-Squares (WLS) | Medium | No | Underestimated [3] | Better than OLS, but not optimal. |
| Generalized Least-Squares (GLS) | High (Theoretical Max) | Yes | Accurate [3] | Highly recommended. |
| Bayesian Regression | High (Theoretical Max) | Yes | Accurate (full posterior) [3] | Highly recommended for uncertainty quantification. |
Table 3: Experimental Techniques for Measuring Drug Diffusion Coefficients
| Experimental Technique | Key Principle | Typical Measurement Time | Reported Diffusion Coefficients (cm²/s) |
|---|---|---|---|
| UV Imaging [105] | Maps 2D drug concentration via UV absorbance; fits Fick's second law. | Minutes (e.g., <10 min) | Carbamazepine: ~7.4x10-6; Ibuprofen: ~7.05x10-6 [105] |
| ATR-FTIR [87] | Tracks drug diffusion by time-resolved IR spectroscopy and Beer's Law. | Hours | Theophylline: 6.56x10-6; Albuterol: 4.66x10-6 (in artificial mucus) [87] |
| Fluorescence Correlation Spectroscopy (FCS) [106] | Analyzes fluorescence intensity fluctuations from a small volume. | Seconds to minutes | Accuracy depends on concentration, molecular brightness, and total measurement time [106] |
Experimental Protocols
Protocol 1: Determining Drug Diffusion Coefficient and Solubility via UV Imaging [105]
This protocol allows for the simultaneous measurement of a drug's diffusion coefficient and solubility.
- Sample Preparation: Prepare a compact of the solid drug. Use double-distilled water or a buffer solution (e.g., phosphate buffer at a specific pH) as the dissolution medium.
- Setup: Place the drug compact at the bottom of a quartz cell. Ensure the system is under static conditions to prevent convective flow.
- Data Acquisition: Use the UV imaging system to record a series of images (UV absorption maps) of the area above the drug compact at constant time intervals. The drug's concentration is directly proportional to its UV absorbance.
- Data Fitting: Fit the obtained 2D concentration profiles over time to a numerical solution of Fick's second law of diffusion.
- Output: The fitting procedure simultaneously yields the diffusion coefficient (D) and the saturation solubility (C_s) of the drug.
Protocol 2: Measuring Drug Diffusion Through Artificial Mucus via ATR-FTIR [87]
This protocol is suited for studying drug transport in biologically relevant barriers like mucus.
- Cell Preparation: Create a thin layer of artificial mucus on the surface of a Zinc Selenide (ZnSe) crystal, which serves as the ATR element.
- Diffusion Initiation: Place a drug solution in contact with the upper surface of the mucus layer.
- Spectra Collection: Collect FTIR spectra at the crystal-mucus interface at constant time intervals. Monitor changes in the height of spectral peaks unique to the drug's functional groups.
- Concentration Calibration: Correlate the peak heights to concentration using Beer's Law.
- Data Analysis: Analyze the concentration-time data using Fick's second law, often with Crank's trigonometric series solution for a planar semi-infinite sheet, to determine the diffusion coefficient.
The Scientist's Toolkit
Table 4: Essential Research Reagents and Solutions
| Item | Function/Application | Example from Literature |
|---|---|---|
| Artificial Mucus | A synthetic construct used to model the complex, hydrophobic mucosal barrier for drug diffusion studies [87]. | Used to measure diffusivity of Theophylline and Albuterol [87]. |
| Phosphate Buffered Saline (PBS) at various pH | To simulate physiological conditions and study the pH-dependent diffusion of ionizable drugs [87]. | Used to measure ibuprofen diffusion at pH 6.5 and 7.5 [87]. |
| Carbamazepine Forms (Anhydrous & Dihydrate) | A model poorly water-soluble drug used in diffusion and dissolution method development [105]. | Used to validate UV imaging for simultaneous solubility and diffusivity measurement [105]. |
kinisi Python Package [3] |
An open-source software tool for the optimal estimation of diffusion coefficients from MSD data using Bayesian regression. | Used to achieve statistically efficient estimates of D* and accurate uncertainty from molecular dynamics simulations [3]. |
andi-datasets Python Package [104] |
A software library to generate simulated single-particle trajectories for benchmarking and training analysis methods. | Used to create the benchmark datasets for the 2nd AnDi Challenge [104]. |
Workflow and Method Diagrams
MSD Analysis Decision Workflow
Experimental Techniques for Diffusion Measurement
Troubleshooting Guides
Guide 1: Resolving Data Quality and Artifact Issues in DTI Acquisition
Problem: Inconsistent or physiologically implausible Mean Diffusivity (MD) and Fractional Anisotropy (FA) values, poor correlation with traditional experimental results (e.g., electrophysiology).
Symptoms:
- FA values are abnormally low or show high variability between similar tissue regions [107]
- MD values do not correlate with established clinical scores or electrophysiological measurements [108]
- High noise levels in Diffusion Weighted (DW) images affecting tensor estimation [107] [109]
Solutions:
- Optimize DTI Acquisition Parameters [109]
- Ensure adequate number of diffusion encoding directions (at least 6, but 30+ recommended for better accuracy)
- Use appropriate b-values (typically 800-1000 s/mm² for brain, 800 s/mm² for peripheral nerves [108])
- Implement readout-segmented EPI (RS-EPI) or multi-shot EPI sequences to reduce geometric distortion [110]
Address Specific Artifact Types [109]
- Eddy current distortion: Use bipolar gradient pulses or post-processing correction methods
- Head motion: Implement prospective motion correction, comfortable head padding, and navigator echoes
- Vibration artifacts: Increase TR or use parallel imaging techniques like GRAPPA
Implement Advanced Denoising Techniques [107]
- Apply deep learning-based denoising (3D DTI-Unet) to improve SNR while maintaining structural details
- Consider traditional methods like MP-PCA or GL-HOSVD when computational resources are limited
- Validate that denoising preserves biological signal integrity through comparison with ground truth data
Guide 2: Addressing Statistical Correlation Failures Between DTI and Traditional Methods
Problem: Lack of statistically significant correlation between DTI parameters (MD, FA, AD, RD) and traditional experimental outcomes.
Symptoms:
- Poor correlation coefficients (r < 0.4) between DTI parameters and functional measurements [108]
- Inconsistent correlation patterns across similar study populations
- DTI parameter changes without corresponding changes in traditional metrics
Solutions:
Cross-Technique Validation Protocols
- Ensure temporal proximity between DTI and traditional measurements (same-day assessment recommended [108])
- Establish a priori correlation thresholds based on pilot studies and previous literature
- Implement blinding procedures for researchers analyzing different modality data
Statistical Power Enhancement
- Conduct sample size calculations using pilot correlation coefficients
- Utilize multiple comparison corrections (FWE, FDR) for voxel-wise analyses [111]
- Consider multivariate approaches that incorporate multiple DTI parameters simultaneously
Frequently Asked Questions
Q1: Our DTI-derived FA values show poor correlation with electrophysiological measurements in ALS patients. What could be causing this?
A: This discrepancy can arise from several factors:
- Spatial mismatch: The DTI ROI may not precisely correspond to the neural pathway being assessed electrophysiologically. Solution: Use fusion techniques combining 3D SHINKEI sequences with DTI for precise anatomical localization [108].
- Timing issues: DTI captures microstructural changes while electrophysiology reflects functional status. Ensure simultaneous assessment and consider disease stage [108].
- Parameter selection: FA alone may be insufficient; include AD and RD to differentiate between axonal damage (reduced AD) and demyelination (increased RD) [108].
Q2: We're getting inconsistent MD values in fetal white matter studies. How can we improve reliability?
A: Inconsistent MD values in developing tissue can be addressed by:
- Controlling for developmental stage: Use precise gestational age matching and consider white matter maturation trajectories [111].
- Implementing advanced processing: Apply TBSS (Tract-Based Spatial Statistics) to align white matter skeletons across subjects [111].
- Accounting for tissue complexity: Use multi-compartment models instead of simple tensor model for highly anisotropic regions [109].
Q3: What are the critical validation steps when correlating DTI findings with traditional histology in animal models?
A: Essential validation steps include:
- Spatial registration precision: Use fiducial markers and high-resolution ex vivo imaging to ensure accurate region matching.
- Parameter-specific hypotheses: Link specific DTI parameters to histological features (e.g., RD with myelin integrity, AD with axonal density) [111] [108].
- Multivariate approaches: Correlate multiple DTI parameters (FA, MD, AD, RD) with quantitative histology measures rather than relying on single parameters.
Experimental Protocols
Protocol 1: DTI Acquisition for Correlation with Electrophysiology
This protocol is optimized for studies correlating DTI parameters with nerve conduction studies, particularly in peripheral nerve applications [108].
Equipment and Setup:
- 3.0T MRI scanner with high-performance gradients (≥40 mT/m)
- Multi-channel phased-array coils appropriate for target tissue
- Compatible electrophysiology equipment for simultaneous or sequential assessment
Step-by-Step Procedure: 1. Subject Preparation - Position subject to minimize motion (comfortable padding, instruction to remain still) - Plan scanning session to immediately precede or follow electrophysiological assessment
- Anatomical Localization
- Acquire high-resolution 3D T1-weighted anatomical images
- Obtain specialized sequences for anatomical reference (e.g., 3D SHINKEI for peripheral nerves [108])
- DTI Acquisition
- Use readout-segmented EPI (RS-EPI) or single-shot EPI with parallel imaging
- Set parameters: TR=6000-9000ms, TE=95ms [111], matrix=256×256 [111]
- Acquire with 32 diffusion encoding directions [108], b=800-1000 s/mm²
- Include multiple b=0 images for reference
- Quality Assessment
- Visually inspect raw DW images for artifacts before subject removal
- Calculate SNR metrics for b=0 images (should be >20 for reliable tensor estimation [107])
Protocol 2: Cross-Technique Correlation Analysis
Standardized methodology for statistically robust correlation between DTI parameters and traditional experimental outcomes.
Data Processing Workflow: 1. DTI Preprocessing - Eddy current correction and motion artifact removal [109] - Tensor reconstruction using robust estimation algorithms (linear least squares or RESTORE [109])
- Parameter Calculation
- Compute primary DTI parameters: FA, MD, AD, RD
- Apply spatial smoothing if using voxel-wise analysis (Gaussian kernel FWHM 2-3x voxel size)
- ROI Definition
- Define ROIs on high-resolution anatomical images
- Transfer ROIs to DTI parameter maps with proper registration
- For tract-based analysis, use TBSS pipeline for skeleton projection [111]
- Statistical Correlation
- Extract mean parameter values from each ROI
- Calculate Pearson or Spearman correlation coefficients with traditional metrics
- Apply multiple comparison correction for family-wise error rate control
DTI Parameters and Their Correlations with Traditional Metrics
Table 1: DTI Parameter Interpretation in Pathological Conditions
| DTI Parameter | Biological Significance | Change in Pathology | Correlation with Traditional Metrics | Typical Correlation Coefficient Range |
|---|---|---|---|---|
| FA (Fractional Anisotropy) | White matter integrity/organization | Decreased in FGR [111], ALS [108] | Positive with ALSFRS-R [108], electrophysiology CMAP amplitude [108] | r = 0.604-0.747 [108] |
| MD (Mean Diffusivity) | Overall water diffusion restriction | Increased in fetal white matter injury [111] | Variable correlation depending on tissue characteristics | Generally weaker than FA [108] |
| AD (Axial Diffusivity) | Axonal integrity | Decreased in ALS (axonal damage) [108] | Positive with nerve conduction velocities [108] | r = 0.480-0.777 [108] |
| RD (Radial Diffusivity) | Myelin integrity | Increased in FGR [111], ALS (demyelination) [108] | Negative with nerve conduction velocities [108] | r = -0.415 to -0.753 [108] |
Table 2: Troubleshooting Common DTI Correlation Problems
| Problem | Potential Causes | Solution Approaches | Validation Method |
|---|---|---|---|
| Poor FA-electrophysiology correlation | ROI misplacement, disease stage mismatch | Anatomical fusion techniques, disease staging stratification | Pilot study with healthy controls |
| Inconsistent MD values across subjects | Motion artifacts, partial volume effects | Rigorous motion correction, higher resolution acquisition | Test-retest reliability analysis |
| Significant but weak correlations | Insensitive traditional metrics, limited sample size | Multimodal assessment, power analysis for sample size | Bootstrap confidence intervals |
| Directionally unexpected correlations | Improper parameter interpretation, confounding factors | Literature review of parameter meanings, covariate analysis | Control experiments with known outcomes |
Experimental Workflow Visualization
DTI Correlation Analysis Workflow
DTI Parameter Correlation Relationships
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for DTI Correlation Studies
| Resource Category | Specific Tool/Technique | Primary Function | Application Notes |
|---|---|---|---|
| Image Acquisition | Readout-Segmented EPI (RS-EPI) | Reduces geometric distortion in DWI [110] | Particularly valuable for high-resolution DTI |
| Simultaneous Multi-Slice (SMS) Acquisition | Accelerates DTI acquisition [110] | Enables higher resolution or more directions within feasible scan time | |
| 3D SHINKEI Sequences | Provides high-resolution nerve visualization [108] | Essential for precise ROI placement in peripheral nerve studies | |
| Data Processing | 3D DTI-Unet (Deep Learning) | Denoises DW images and estimates diffusion tensors [107] | Superior to MP-PCA and GL-HOSVD for limited direction data [107] |
| FSL TBSS Pipeline | Enables voxel-wise analysis of white matter skeleton [111] | Standardized approach for multi-subject DTI studies | |
| Eddy Current Correction | Corrects distortion from diffusion gradients [109] | Critical for accurate tensor estimation | |
| Statistical Analysis | Tract-Based Spatial Statistics | Group-wise white matter analysis [111] | Minimizes alignment issues in multi-subject studies |
| Multiple Comparison Correction (FWE/FDR) | Controls false positive rates [111] | Essential for voxel-wise correlation analyses | |
| Multivariate Regression Models | Analyzes multiple DTI parameters simultaneously | Captures complex structure-function relationships |
This section provides a consolidated overview of key quantitative findings from recent studies on Apparent Diffusion Coefficient (ADC) and Diffusion Tensor Imaging (DTI) for prostate cancer (PCa) diagnosis.
Table 1: Diagnostic Performance of ADC and DTI Parameters in Prostate Cancer
| Parameter | Cancer vs. Benign Tissue Finding | Diagnostic Performance (AUC/Accuracy) | Key Clinical Utility |
|---|---|---|---|
| ADC Value | Significantly lower in PCA [112] | Combined T2WI+DWI AUC: 0.902 [112] | Distinguishes cancerous tissue; correlates with tumor cellularity [113]. |
| DTI - λ1 (Prime Diffusion Coefficient) | Significantly lower in PCa (PZ and CG) [114] | PPV: 77.8%; NPV: 91.7% [114] | Improves cancer detection without contrast injection [114]. |
| DTI - FA (Fractional Anisotropy) | Distinguishes PCa lesions from normal tissue [114] | Model with multiple DTI parameters shows improved sensitivity/specificity [114] | Reflects microstructural tissue disruption [114]. |
| VERDICT - fic (Intracellular Volume) | Higher in clinically significant PCa [115] | AUC for discriminating Gleason 3+3 vs 3+4: 0.93 [115] | Provides specific histologic correlation with epithelial volume [115]. |
| PSMA-PET | More sensitive than mpMRI/CT/BS [116] | Nodal Staging Sensitivity: 73.7% (vs. mpMRI 38.9%) [116] | Superior for initial staging of intermediate-high risk PCa [116]. |
Table 2: Typical Parameter Values in Prostate Cancer versus Benign Tissue
| Metric | Typical Value in Prostate Cancer | Typical Value in Benign Tissue | Primary Biological Meaning |
|---|---|---|---|
| ADC ( [112]) | ( 0.75 \pm 0.15 \times 10^{-3} \, \text{mm}^2/\text{s} ) (example) | ( 1.02 \pm 0.21 \times 10^{-3} \, \text{mm}^2/\text{s} ) (example) | Measure of water diffusion magnitude; inversely related to tissue cellularity [112] [113]. |
| λ1 (Principal Diffusion) ( [114]) | Lower | Higher | Diffusion rate along the primary axis; restricted in cancer [114]. |
| FA (Anisotropy) ( [114]) | Varies | Varies | Degree of directional water diffusion; reflects tissue microstructure integrity [114]. |
| T2 Relaxation ( [115]) | Shorter | Longer | Altered in cancerous tissue; can be modeled jointly with diffusion [115]. |
Experimental Protocols
This section details standard methodologies for key experiments involving ADC and DTI in prostate cancer research.
Multiparametric MRI (mpMRI) Protocol for Prostate Cancer
This protocol is based on a retrospective diagnostic study [112].
- Patient Preparation: No requirement for bladder filling prior to the examination [112].
- Scanner and Hardware: MRI system (e.g., 1.5T or 3T, such as SIEMENS Altea 1.5T) equipped with a phased-array abdominal coil [112].
- Pulse Sequences and Key Parameters:
- T2-Weighted Imaging (T2WI): Fast spin-echo (FSE) sequence in axial, sagittal, and coronal planes. Example Parameters: TR: 3420 ms, TE: 98 ms, Slice thickness: 5 mm, Gap: 1 mm, FOV: 24x24 cm [112].
- Diffusion-Weighted Imaging (DWI): Axial single-shot echo-planar imaging (EPI) sequence. Example Parameters: TR: 3200 ms, TE: 84 ms, Matrix: 256x256, Slice thickness: 3 mm, Gap: 0.3 mm. Use multiple b-values (e.g., b=50 and b=800 s/mm²) for ADC calculation [112].
- Dynamic Contrast-Enhanced (DCE) MRI: Volumetric T1-weighted sequence (e.g., LAVA) before and after contrast administration. Example Parameters: TR: 145 ms, TE: 4.76 ms, Slice thickness: 5 mm. Inject gadolinium-based contrast agent (e.g., gadobutrol, 0.1 mL/kg) intravenously at 2.5 mL/s, initiating dynamic scanning during injection [112].
- Data Analysis:
Diffusion Tensor Imaging (DTI) Protocol for Prostate Cancer
This protocol is adapted from a pilot study investigating DTI for PCa detection [114].
- Scanner and Hardware: 3T MRI scanner (e.g., Philips Ingenia) using a multi-channel torso coil [114].
- DTI Sequence:
- Type: 2D axial spin-echo, echo-planar imaging (EPI).
- Key Parameters: Diffusion gradients applied in 32 directions; two b-values (e.g., b=0 and b=600 s/mm²); TR/TE: ~4163/70 ms; slice thickness: 3 mm with 0.3 mm gap; in-plane resolution: ~1.43x1.43 mm. The sequence is performed before contrast injection [114].
- Data Processing and Analysis:
- Software: Use dedicated DTI processing software (e.g., custom solutions like DDE MRI Solution Ltd. or FSL/TORTOISE for research) [114].
- Tensor Calculation: The software calculates a symmetric diffusion tensor for each voxel, yielding three eigenvectors (directions) and three eigenvalues (λ1, λ2, λ3) - the directional diffusion coefficients [114].
- Metric Calculation:
- ROI Analysis: Generate parametric maps (λ1, λ2, λ3, MD, FA, MA). Manually or semi-automatically draw ROIs on cancerous lesions (based on T2WI and reference standard) and normal-appearing tissue to extract mean values for each metric [114].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for ADC/DTI Prostate Cancer Research
| Item | Function / Explanation | Example/Note |
|---|---|---|
| 3T MRI Scanner | High-field strength provides superior signal-to-noise ratio (SNR) and spatial resolution for discerning subtle prostate lesions. | Essential for advanced techniques like DTI [114]. |
| Multi-Channel Phased-Array Coil | A surface coil placed over the area of interest to improve SNR for prostate imaging. | E.g., 32-channel posterior/anterior torso coils [114]. |
| Gadolinium-Based Contrast Agent | Used in DCE-MRI to assess tissue vascularity and permeability. | E.g., Gadobutrol. Not required for biparametric MRI (bpMRI) or DTI-only protocols [112] [113]. |
| DTI Processing Software | Specialized software is required to compute the diffusion tensor and derive anisotropy metrics (FA, MD, λ1-3). | Commercial or in-house solutions (e.g., DDE MRI Solution Ltd.) [114]. |
| Biopsy Validation System | Gold standard for validating imaging findings. MRI-targeted biopsies improve accuracy. | E.g., UroNav fusion system for combining MRI and ultrasound images during biopsy [112]. |
| rVERDICT Model | An advanced biophysical model that jointly estimates diffusion and relaxation parameters for improved Gleason grade discrimination. | Research technique showing high AUC for discriminating cancer grades [115]. |
Visualization of Workflows and Relationships
MRI Analysis Pathway
Parameter Relationship Logic
Troubleshooting Guides and FAQs
Q1: We are observing high variability and poor repeatability in our DTI metrics (FA, λ1). What could be the root causes and solutions?
A: Poor DTI repeatability often stems from technical and physiological factors.
- Root Causes:
- Insufficient Number of Diffusion Directions: Using too few directions (e.g., less than 20) can lead to inaccurate tensor estimation. Solution: Increase the number of encoding directions to 30-32 for robust tensor calculation [114].
- Low Signal-to-Noise Ratio (SNR): This is critical for DTI. Solution: Ensure use of a 3T scanner and a multi-channel phased-array coil. If possible, increase the number of averages, though this lengthens scan time [114].
- Patient Motion: Even slight movement can corrupt DTI data. Solution: Use comfortable immobilization and instruct the patient on the importance of staying still. Consider using a rectal balloon for prostate immobilization if compatible with your protocol.
- Magnetic Field Inhomogeneity: Can distort EPI-based DTI. Solution: Ensure proper shimming is performed over the region of interest prior to the DTI sequence [118].
Q2: Our calculated ADC values for confirmed prostate cancer lesions overlap significantly with values from benign prostatic hyperplasia (BPH) or prostatitis. How can we improve specificity?
A: Overlap is a known challenge, as conditions like prostatitis also increase cellularity, reducing ADC.
- Solutions:
- Incorporate DTI Metrics: Use DTI in conjunction with ADC. The prime diffusion coefficient (λ1) has shown higher Positive Predictive Value (PPV) and Negative Predictive Value (NPV) than standard mpMRI in some studies, potentially offering better specificity [114].
- Use Advanced Models: Employ biophysical models like rVERDICT. This model jointly estimates diffusion and relaxation parameters, and its intracellular volume fraction (fic) has demonstrated superior discrimination between Gleason grades compared to ADC alone, potentially reducing false positives from BPH [115].
- Correlate with Anatomy: Always interpret ADC values in the context of high-resolution T2-weighted images. The location and morphology of the lesion (e.g., in the transition or peripheral zone) are critical for accurate diagnosis [112] [117].
Q3: What are the critical steps for validating that our DTI-derived parameters accurately reflect underlying prostate tissue microstructure?
A: Robust validation is essential for translating DTI biomarkers into clinical research.
- Critical Steps:
- Histopathologic Correlation: This is the gold standard. Correlate DTI parameter maps from pre-biopsy MRI with whole-mount prostatectomy specimens using sophisticated 3D coregistration techniques. For biopsy-based validation, ensure accurate spatial matching between the biopsy core location (e.g., via MRI-US fusion systems) and the ROI on the DTI map [112] [115].
- Test-Retest Repeatability: Perform a scan-rescan study in a subset of patients to quantify the repeatability of your DTI metrics. Report metrics like the Intraclass Correlation Coefficient (ICC) and Coefficient of Variation (CV). High repeatability (e.g., ICC >0.9, CV <10%) is a strong indicator of reliability [115].
- Comparison to Established Standards: Benchmark your DTI results against the diagnostic performance of ADC and PI-RADS v2.1 scores from standard mpMRI, using histopathology as the reference standard [114].
Q4: How can we effectively integrate ADC and DTI data into a single diagnostic model without overcomplicating the clinical workflow?
A: Integration is key to leveraging the strengths of both techniques.
- Effective Integration Strategies:
- Develop a Machine Learning Classifier: Use a Random Forest or Support Vector Machine (SVM) model. Input features should include ADC mean value, DTI metrics (λ1, FA), and potentially standard PI-RADS scores and clinical data (e.g., PSA). This can output a single, optimized risk score for clinically significant cancer [117].
- Create a Sequential Reading Protocol: In a clinical workflow, a radiologist could first assess the standard mpMRI (T2WI, DWI, ADC) and assign a PI-RADS score. For indeterminate cases (e.g., PI-RADS 3), the DTI parametric maps (especially λ1) can be consulted as a "tie-breaker" to increase diagnostic confidence [114].
- Adopt Biparametric MRI (bpMRI) with DTI: To streamline the protocol, consider a bpMRI approach (T2WI + DWI/ADC) and replace the contrast-enhanced (DCE) sequence with the DTI acquisition. This maintains a short scan time while adding valuable microstructural information from DTI [113] [114].
Conclusion
The accurate estimation of diffusion coefficients is contingent upon a rigorous statistical approach that acknowledges and quantifies uncertainty. This synthesis of foundational principles, advanced methodological approaches, robust error analysis, and thorough validation provides a clear path for researchers to enhance the reliability of their diffusion data. The move beyond simple linear regression to more sophisticated methods like Bayesian and generalized least-squares regression is crucial for obtaining statistically efficient and unbiased estimates. Future progress in biomedical research, particularly in the development of targeted drug delivery systems and the clinical application of diffusion-based imaging, will be increasingly dependent on these high-fidelity measurements. Embracing standardized error reporting and open-source analysis tools will be key to improving reproducibility and driving innovation in the field.
References
- 1. Diffusion coefficient — Tutorials 2025.1 documentation - SCM [https://www.scm.com/doc/Tutorials/MolecularDynamicsAndMonteCarlo/BatteriesDiffusionCoefficients.html]
- 2. How are diffusion coefficients calculated? [https://mattermodeling.stackexchange.com/questions/9224/how-are-diffusion-coefficients-calculated]
- 3. Accurate Estimation of Diffusion Coefficients and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11736684/]
- 4. Maximum likelihood-based estimation of diffusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10031098/]
- 5. [2003.09193] Optimal estimates of diffusion coefficients ... [https://arxiv.org/abs/2003.09193]
- 6. Resolving experimental biases in the interpretation of ... [https://www.nature.com/articles/s41598-023-42260-5]
- 7. Ensemble-Based Correction for Anomalous Diffusion ... [https://www.mdpi.com/2076-3417/15/14/8000]
- 8. Lesson 8 Statistical uncertainty | Data Science in R [https://bookdown.org/jgscott/DSGI/statistical-uncertainty.html]
- 9. Insights into the quantification and reporting of model-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9712693/]
- 10. Multi-institution longitudinal apparent diffusion coefficient ... [https://pubmed.ncbi.nlm.nih.gov/40755885/]
- 11. Tracking Molecular Diffusion across Biomaterials' Interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9305705/]
- 12. Synthetic Data from Diffusion Models Improve Drug ... [https://arxiv.org/abs/2405.03799]
- 13. Mean squared displacement [https://en.wikipedia.org/wiki/Mean_squared_displacement]
- 14. Apparent Diffusion Coefficient - an overview [https://www.sciencedirect.com/topics/immunology-and-microbiology/apparent-diffusion-coefficient]
- 15. TRAIT2D: a Software for Quantitative Analysis of Single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8829092/]
- 16. Assessing the ADC of Bone-marrow on Whole-body MR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9316130/]
- 17. Focus on Diffusion MR Investigations of Musculoskeletal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4377366/]
- 18. A multicenter phantom study using multi-point b-values [https://www.sciencedirect.com/science/article/abs/pii/S1078817424003407]
- 19. Why Your ADC Measurements Are Inaccurate [https://runtimerec.com/why-your-adc-measurements-are-inaccurate-common-pitfalls-and-fixes/]
- 20. Estimation of covariance matrices [https://en.wikipedia.org/wiki/Estimation_of_covariance_matrices]
- 21. Confidence interval [https://en.wikipedia.org/wiki/Confidence_interval]
- 22. Basic statistical tools in research and data analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5037948/]
- 23. Which Statistical Software to Use? - Quantitative Analysis ... [https://guides.nyu.edu/quant/statsoft]
- 24. Common errors when using GROMACS [https://manual.gromacs.org/2024.4/user-guide/run-time-errors.html]
- 25. Avoiding Common Mistakes When Setting Up a Production MD ... [https://blog.samson-connect.net/avoiding-common-mistakes-when-setting-up-a-production-md-simulation]
- 26. 10 Common Molecular Dynamics Mistakes New ... [https://insilicosci.com/common-molecular-dynamics-mistakes/]
- 27. 4.7.2.2. Mean Squared Displacement [https://docs.mdanalysis.org/2.7.0/documentation_pages/analysis/msd.html]
- 28. Is MSD increasing too fast? What's wrong? [https://forum.image.sc/t/is-msd-increasing-too-fast-whats-wrong/90886]
- 29. Mean Square Displacement Analysis of Single-Particle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3055791/]
- 30. Bayesian Statistics: A Modern Data Analysis in 2025 [https://clinilaunchresearch.in/guide-to-bayesian-statistics/]
- 31. Bayesian Logistic Regression Model (BLRM) [https://www.precisionformedicine.com/blog/phase-1-clinical-trial-design-bayesian-logistic-regression-model]
- 32. Global burden and trends of musculoskeletal disorders in ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-025-03587-8]
- 33. A state-of-the-art review of Bayesian finite element model ... [https://www.sciencedirect.com/science/article/abs/pii/S0266892025000335]
- 34. Using Bayesian statistics in confirmatory clinical trials in the ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02235-0]
- 35. Bayesian Approach to MSD-Based Analysis of Particle ... [https://www.sciencedirect.com/science/article/pii/S0006349512007187]
- 36. Bayesian data-driven models for pharmaceutical process ... [https://www.sciencedirect.com/science/article/abs/pii/S2211339824000352]
- 37. Application of Bayesian approaches in drug development [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931171/]
- 38. Taylor Dispersion Analysis (TDA) Introduction and Overview [https://www.azom.com/article.aspx?ArticleID=12173]
- 39. Taylor Dispersion Analysis (TDA) in DSBC group [https://ibmm.umontpellier.fr/dsbc/tda_en.html]
- 40. Taylor Dispersion Analysis of Mixtures [https://nanoscale-metrix.com/ressources/taylor-dispersion-analysis-of-mixtures/]
- 41. Taylor Dispersion Analysis and Size-Based ... [https://www.nature.com/research-intelligence/nri-topic-summaries/taylor-dispersion-analysis-and-size-based-characterization-techniques-micro-273687]
- 42. Taylor dispersion [https://en.wikipedia.org/wiki/Taylor_dispersion]
- 43. Methodologies for the rapid determination of the diffusion ... [https://pubs.rsc.org/en/content/articlelanding/2016/ay/c5ay02614h]
- 44. Everything You Need to Know About ATR-FTIR Spectroscopy [https://specac.com/everything-you-need-to-know-about-atr-ftir-spectroscopy/]
- 45. Measuring diffusion coefficients with ATR-FTIR [https://www.linkedin.com/posts/profstevenabbott_diffusion-coefficients-via-atr-ftir-people-activity-7392475365698535424-RbVI]
- 46. Advances in ATR-FTIR Spectroscopic Imaging for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10301043/]
- 47. Use of ATR-FTIR spectroscopy to study the diffusion ... [https://pubmed.ncbi.nlm.nih.gov/7596994/]
- 48. Operando FTIR-ATR with molecular dynamic simulations to ... [https://www.sciencedirect.com/science/article/abs/pii/S0016236123024481]
- 49. FT-IR Troubleshooting Guide: How to Solve Common ... [https://www.spectroscopyonline.com/view/ftir-troubleshooting-guide-how-to-solve-common-problems-in-infrared-spectroscopy]
- 50. Common Problems with FT-IR Instruments and How to ... [https://www.spectroscopyonline.com/view/common-problems-with-ft-ir-instruments-and-how-to-avoid-them]
- 51. Application of ATR-FTIR spectroscopy and multivariate ... [https://www.sciencedirect.com/science/article/pii/S2472630325000111]
- 52. Reduction of systematic errors in diffusion tensor imaging ... [https://www.sciencedirect.com/science/article/pii/S0010482525008546]
- 53. Apparent diffusion coefficient as a quantitative biomarker ... [https://www.sciencedirect.com/science/article/pii/S2405631625001563]
- 54. Advanced breast diffusion-weighted imaging - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11914331/]
- 55. The ins and outs of errors in oncology imaging - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11486622/]
- 56. Early Prediction of Radiotherapy Outcome Using ADC ... [https://www.sciencedirect.com/science/article/pii/S0360301625017481]
- 57. Correlation between apparent diffusion coefficient (ADC) and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601748/]
- 58. Comparative analysis of apparent diffusion coefficient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11987170/]
- 59. Current Applications of Diffusion Tensor Imaging and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6549594/]
- 60. Diffusion-tensor imaging as an adjunct to dynamic contrast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4409968/]
- 61. Diffusion-tensor imaging as an adjunct to dynamic contrast ... [https://www.cjcrcn.org/article/6226.html]
- 62. Standard Error vs Standard Deviation: Finding the Difference [https://www.6sigma.us/six-sigma-in-focus/standard-error-vs-standard-deviation/]
- 63. Standard deviations and standard errors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1255808/]
- 64. The SD and SEM are not the same [https://www.graphpad.com/guides/prism/latest/statistics/stat_semandsdnotsame.htm]
- 65. differences between the standard deviation and ... [https://pubmed.ncbi.nlm.nih.gov/8899234/]
- 66. Standard error [https://en.wikipedia.org/wiki/Standard_error]
- 67. When to Report the Standard Deviation vs. the Standard Error [https://www.biostatisticsbydesign.com/blog/2019/1/5/when-to-report-the-standard-deviation-vs-the-standard-error]
- 68. Standard Deviation vs. Standard Error: Meaning, Misuse ... [https://www.r-bloggers.com/2025/07/standard-deviation-vs-standard-error-meaning-misuse-and-the-math-behind-the-confusion/]
- 69. Standard Error Meaning [https://byjus.com/maths/standard-error/]
- 70. Variance, Standard Deviation and Standard Error - LibGuides ... [https://library.soton.ac.uk/variance-standard-deviation-and-standard-error]
- 71. Subdiffusive-Brownian crossover in membrane proteins [https://pmc.ncbi.nlm.nih.gov/articles/PMC8595736/]
- 72. Subdiffusion in Membrane Permeation of Small Molecules [https://www.nature.com/articles/srep35913]
- 73. Prediction and validation of diffusion coefficients in a model ... [https://pubs.rsc.org/en/content/articlelanding/2014/sm/c4sm01297f]
- 74. Diffusion FAQ: The basics [https://physicallensonthecell.org/diffusion-faq-basics]
- 75. A compact guide to performing Molecular Dynamics ... [https://www.sciencedirect.com/science/article/pii/S0167273825001869]
- 76. Quantitative evaluation of apparent diffusion coefficient in a ... [https://www.sciencedirect.com/science/article/pii/S2405631625001617]
- 77. Understanding Ordinary Least Squares (OLS) Regression [https://builtin.com/data-science/ols-regression]
- 78. 7 Classical Assumptions of Ordinary Least Squares (OLS ... [https://statisticsbyjim.com/regression/ols-linear-regression-assumptions/]
- 79. The importance of measuring diffusion coefficients in ... [https://pubs.rsc.org/en/content/articlelanding/2025/ra/d5ra00669d]
- 80. Study on the self-diffusion coefficients of binary mixtures ... [https://www.sciencedirect.com/science/article/abs/pii/S004313542500764X]
- 81. Generalized least squares [https://en.wikipedia.org/wiki/Generalized_least_squares]
- 82. Analysis of Structural Health Monitoring Data with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9609834/]
- 83. Heteroskedasticity and Serial Correlation - CFA, FRM, and ... [https://analystprep.com/study-notes/cfa-level-2/quantitative-method/heteroskedasticity-serial-correlation/]
- 84. Heteroskedasticity and Autocorrelation simply explained [https://www.finance-tutoring.fr/heteroskedasticity-and-autocorrelation-simply-explained]
- 85. Autocorrelation and heteroskedasticity in time series data [https://stats.stackexchange.com/questions/313452/autocorrelation-and-heteroskedasticity-in-time-series-data]
- 86. A joint test for serial correlation and heteroscedasticity in ... [https://www.sciencedirect.com/science/article/abs/pii/S0165176520303578]
- 87. Experimental and modeling approaches to determine drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11619999/]
- 88. Diffusion coefficients of an extensive set of pharmaceutical ... [https://www.sciencedirect.com/science/article/abs/pii/S0021967322005209]
- 89. Molecular Modeling to Estimate the Diffusion Coefficients ... [https://www.mdpi.com/1420-3049/25/22/5340]
- 90. Part 1: Single Moving Average and Error Estimation [https://medium.com/@polanitzer/time-series-methodologies-part-1-single-moving-average-and-error-estimation-34b6518797a8]
- 91. Time Series Forecast Error Metrics you should know [https://towardsdatascience.com/time-series-forecast-error-metrics-you-should-know-cc88b8c67f27/]
- 92. Validation technique could help scientists make more ... [https://news.mit.edu/2025/validation-technique-could-help-scientists-make-more-accurate-forecasts-0207]
- 93. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 94. Data validation: techniques, challenges and best practices [https://www.future-processing.com/blog/data-validation/]
- 95. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 96. Error Analysis [https://erroranalysis.ai/]
- 97. Estimation of diffusion coefficients in NiCoFeCrAl multi ... [https://www.sciencedirect.com/science/article/abs/pii/S1359645423006262]
- 98. How Statistical Regressions Learn to Trust: OLS , WLS , and GLS in... [https://pub.towardsai.net/how-statistical-regressions-learn-to-trust-ols-wls-and-gls-in-action-44b1802097a3]
- 99. How to choose between different methods of linear regression ? [https://stats.stackexchange.com/questions/476867/how-to-choose-between-different-methods-of-linear-regression]
- 100. Advantages vs. disadvantages of Bayesian statistics [https://www.linkedin.com/pulse/advantages-vs-disadvantages-bayesian-statistics-miguel-pereira-md-phd]
- 101. Bayesian Linear Regression vs Least Squares [https://stats.stackexchange.com/questions/554065/bayesian-linear-regression-vs-least-squares]
- 102. Objective comparison of methods to decode anomalous ... [https://arxiv.org/html/2105.06766v2]
- 103. Measuring a diffusion coefficient by single-particle tracking [https://pubs.rsc.org/en/content/articlelanding/2013/cp/c2cp43433d]
- 104. Quantitative evaluation of methods to analyze motion ... [https://www.nature.com/articles/s41467-025-61949-x]
- 105. Simultaneous Rapid Determination of the Solubility and ... [https://www.sciencedirect.com/science/article/abs/pii/S0022354915001367]
- 106. Statistical Analysis of Diffusion Coefficient Determination ... [https://link.springer.com/article/10.1007/s10895-005-2633-0]
- 107. 基于3D U-Netå’ŒDTI模型约æŸçš„æ‰©æ•£å¼ é‡åœºä¼°è®¡æ–¹æ³• [https://pmc.ncbi.nlm.nih.gov/articles/PMC10366516/]
- 108. åŸºäºŽæ‰©æ•£å¼ é‡æˆåƒçš„è‚ŒèŽç¼©ä¾§ç´¢ç¡¬åŒ–症臂丛神ç»æ ¹å¾®è§‚结构 ... [https://www.ebiotrade.com/newsf/2025-11/20251115050645484.htm]
- 109. Frontiers in Neuroscienceï¼šå¼¥æ•£å¼ é‡æˆåƒ(DTI)ç ”ç©¶æŒ‡å— [http://www.syfmri.cn/Service/info/id/94.html]
- 110. Review of high-resolution 2-dimensional diffusion ... [https://wulixb.iphy.ac.cn/en/article/doi/10.7498/aps.74.20250235?viewType=HTML]
- 111. Quantitative evaluation of white matter development in fetus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7390043/]
- 112. Analysis of the Diagnostic Efficacy and Clinical Utility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399885/]
- 113. MRI apparent diffusion coefficient (ADC): A biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9612745/]
- 114. Innovative Diffusion Tensor Imaging to Improve Prostate ... [https://www.mdpi.com/2075-4418/11/3/563]
- 115. Joint estimation of relaxation and diffusion tissue ... [https://www.nature.com/articles/s41598-023-30182-1]
- 116. to High-risk Prostate Cancer: A Systematic Review and ... [https://pubmed.ncbi.nlm.nih.gov/37032189/]
- 117. Integration of magnetic resonance imaging and deep learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12089223/]
- 118. Diffusion Tensor Imaging (DTI) as a Nonâ€Invasive Tool for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12159281/]